The Embryo Bank Dilemma: Reviewing the Issues, Historical Perspectives and Offering Potential Solutions

Craig R. Sweet, M.D
Reproductive Endocrinologist
Practice and Medical Director
Embryo Donation International
Introduction
In my last blog, “Why Creating ‘McEmbryos’ is Just Plain Wrong,” I wrote about my concerns regarding the creation of an embryo bank at a California clinic. In this follow-up segment, I want to re-state the issues, discuss the past history of embryo banking in the U.S., provide a list of recently written thoughtful blogs on the topic, offer possible solutions to the dilemma and discuss where we should go from here.
A “Reader’s Digest” version
California Conceptions (CC), as outlined in Alan Zarembo’s L.A. Times article apparently combined donor eggs with donor sperm and divided the resulting embryos among a number of embryo recipients. This process is commonly called a “split or shared donor/donor cycle” but was called “embryo donation” by CC. Any embryos remaining, after the recipients received their allotment, would be cryopreserved and owned by CC.
The road was paved with good intentions
I feel that CC was really trying to offer a cost-affective alternative for patients and that its true intent was to keep the size of its embryo bank as small as possible. Even with good intentions, however, it is quite likely that the embryo bank will grow. In addition, to sanction the creation of a small embryo bank will almost certainly result in the creation of larger embryo banks across the country. These banked embryos for commercial use are what I called “McEmbryos.” There also needs to be a clear distinction between embryo banking for commercial use and the process of banking one’s own embryos (i.e., collecting through multiple IVF retrievals) to be used by individuals to build their families in the future.
I still have three main concerns:
- I do not feel that embryo banks are appropriate and could result in a plethora of unintended consequences.
- I feel that corporations, businesses or physician practices should not own embryos.
- Lastly, the process of a “split or shared donor/donor cycle” should be called “embryo creation” or, at the very least, not called embryo donation.
This has happened before
An article by Gina Kolata in the New York Times in 1997 revealed that “ready-made embryos” were already being made for “adoption.” Columbia-Presbyterian and Reproductive Biology Associates were named in the article as providing “premade” embryos to patients. According to the article, most of the embryos were created when donor egg recipients backed out of the process, but the egg donors still underwent the egg retrieval; their subsequent retrieved donor oocytes were combined with donor sperm. Lori B. Andrews, a professor of law at Chicago-Kent College of Law, was quoted as having concerns about the supermarket approach to embryos while the clinicians thought it wasteful to not retrieve and fertilize the donor oocytes if the egg donors were ready for the retrieval.
In 2007, Center for Genetics and Society Senior Fellow and UC Hastings Law Professor Osagie Obasogie wrote an op-ed for the Boston Globe about a Texas center that had created an embryo bank. He was concerned about the “Wal-Martization” of human embryos, a phrase similar to my “McEmbryos.”
In November of 2012, in response to the N.Y. Times article, Jessica Cussins of the Center for Genetics and Society wrote an excellent blog on the topic, also following-up on the 2007 article by Professor Obasogie. The Texas center was eventually closed and was the subject of an FDA investigation, which eventually found that the creation of an embryo bank did not fall under FDA jurisdiction. John Robertson, Esq., wrote an excellent commentary on the topic in the Bioethics Forum in that same year.
Embryo banks have come and gone, garnering media attention and criticism and I believe it is finally time to set some ethical standards of care about them.
How New York decided to handle the embryo bank issue
 Almost five years ago, the state of New York issued regulations for tissue banks and nontransplant anatomic banks, addressing the potential of creating embryo banks:
Almost five years ago, the state of New York issued regulations for tissue banks and nontransplant anatomic banks, addressing the potential of creating embryo banks:
Embryos shall not be created for donation by fertilizing donor oocytes with donor semen, except at the request of a specific patient who intends to use such embryos for her own treatment. [NYS 52-8.7(h)]
Embryos were not to be created to store in embryo banks but only created at the behest of a specific patient and subsequently owned by that patient. Simply modifying the statement above to include “… such embryos for his/her own treatment,” would address the issue adequately, with the sentence potentially used by various organizations as they hopefully set ethical standards of care.
Potential consequences to the creation of an embryo bank
I have been called an alarmist by some for bringing up what I feel are the following potential dangers of having embryos banks in the U.S:
- If a small embryo bank is allowed to flourish, then large embryo banks will most certainly follow.
- Poorly designed and reactive legislation may be created on the state or national level as there may be further calls to regulate what are perceived to be “unregulated IVF facilities.”
- “Personhood” advocates may become further emboldened to win personhood for the embryos to protect them from becoming “McEmbryos.”
I don’t think these unintended consequences are that farfetched and need to be considered carefully should embryo banks continue unchecked.
My reluctant decision to come forward
 About the last thing I wanted to do was to comment on another reproductive endocrine practice comprised of caring staff members dedicated to the care of their patients. I have been criticized for taking such a stand and accused of doing this purely for competitive reasons. In reality, I have been working with the American Society for Reproductive Medicine’s (ASRM) and the Society for Assisted Reproductive Technologies, (SART) since October of 2011, trying to elicit a set of guidelines prior to the writing of my blog. I far preferred to stay out of the limelight and let the “powers-that-be” decide what should be done next. When the L.A. Times article was published, it de-emphasized the ethical issues and potential unintended consequences of the CC embryo banking practice, so I felt I had no choice but to bring the topic up front and center.
About the last thing I wanted to do was to comment on another reproductive endocrine practice comprised of caring staff members dedicated to the care of their patients. I have been criticized for taking such a stand and accused of doing this purely for competitive reasons. In reality, I have been working with the American Society for Reproductive Medicine’s (ASRM) and the Society for Assisted Reproductive Technologies, (SART) since October of 2011, trying to elicit a set of guidelines prior to the writing of my blog. I far preferred to stay out of the limelight and let the “powers-that-be” decide what should be done next. When the L.A. Times article was published, it de-emphasized the ethical issues and potential unintended consequences of the CC embryo banking practice, so I felt I had no choice but to bring the topic up front and center.
Others responded to the discussion
Several other infertility professionals discussed the ethical issue in articles or blogs in the weeks following the L.A. Times piece. Excluding those that simply summarized the situation, I listed below what I think are some of the better blogs:
Supporting embryo banking
- Marni Soupcoff, Esq., “Marni Soupcoff on the sale of fertilized embryos: How much for the blastocyst in the window?”
Neutral to embryo banking
- Julie Shapiro, Esq., “Custom Made or Off The Rack?”
- Carole C. Wegner, Ph.D., “Embryos for Donation: Where are the ethical boundaries?“
- Elizabeth Swire Falker, Esq., “The Bizarre World of Embryo Banking. Where My Motherhood and Morality Meet”
Against embryo banking
- Andrew Vorzimer, Esq., “Get Pregnant With Built On Spec Embryos Or Get Your Money Back!”
- Jessica Cussins, B.A., “Embryos for Sale: ‘When You Want Them, How You Want Them, or Your Money Back”
- Sara R. Cohen, LL.B., “It’s not about the Money: Why we are So Concerned about a California IVF Clinic’s Anonymous Embryo Program”
- Mikki Morrissette, “Creating Embryos To Sell“
My thanks to all of the authors for taking the time to discuss the issue in an open forum.
Proposed remedies to the current dilemma
From the beginning, I have been offering remedies to the embryo bank dilemma. Although far be it from me to tell CC how to run its business, these are a few ideas I had to offer:
Only patients should own embryos-
No organization, corporation or physician practice should own embryos except in the most extreme circumstances, such as embryo abandonment. With embryo donation, it is most appropriate that the donor facility simply holds the embryos, with the donors still being able to request the return of their embryos, up to the point of transfer into the recipients, should a catastrophic occurrence take place, Attorneys refer to this as being a guardian, a conservator, or a temporary holder of goods. When presenting at the American Bar Association Family Law Section Spring conference in April of 2012, many of the attorneys there strongly supported the concept of conservatorship of the donated embryos over facility ownership.
If the embryos are returned to the donor, it seems appropriate to ask the donors to reimburse the embryo donation facility for all reasonable fees expended in originally obtaining the donated embryos and returning them to the donors. We have been running our embryo donation program this way for over 12 years and we encourage others to do the same.
Excess cryopreserved embryos could be owned by patients-
As best as I can surmise for CC, their business model is to recruit a number of embryo recipients and then transfer 1-2 donor/donor embryos into each recipient. I suggest that any remaining embryos be owned by one or more of the recipients and the entire cycle should not move forward until at least one patient agrees to take the extra cryopreserved embryos, should any exist. Extra charges could be levied to those that secure the remaining embryos. In this way, no embryos remain to create an embryo bank and the CC business model remains essentially intact.
Renaming the process-
The combination of donor sperm with donor eggs and then calling them donated embryos does not fit with the ASRM definition of embryo donation (Ethics Committee of the ASRM, 2009). Embryo creation is a far better term or “shared or split donor/donor cycle” is perhaps even more appropriate. Calling such embryos donated embryos debases the amazing gift that embryo donors provide when donating their embryos.
Who should set the standards?
 SART has reviewed the concerns stated in my previous blog but I don’t think it yet has arrived at a
SART has reviewed the concerns stated in my previous blog but I don’t think it yet has arrived at a
conclusion. My understanding is that the ASRM Ethics Committee is to take up the topic during the early months of 2013. As our main guiding societies, I believe they need to take the lead, develop position statements and provide ethical standard of care guidelines for all practices to use.
Once ASRM and SART have provided ethical standard of care guidelines, I will next request that the

Canadian Fertility and Andrology Society and the European Society for Human Reproduction and Embryology (I am a member of both) consider the topic and respond with their own recommendations if they see fit.
It is not out of the realm of possibility that numerous societies could collaborate to form a consensus, such as they did when they banned the support and publication of human reproductive cloning research.
Summary comments
So where are we now on this dilemma? SART has discussed the topic but summary statements are pending. The ASRM Ethics Committee will soon meet, with the embryo bank topic apparently on the agenda. Assuming the Ethics Committee feels the topic has merit, I am uncertain how long it will take for them to release a position statement. I am hopeful that “the powers that be” will be attentive in finding a compromise that will allow CC to continue to offer their skilled reproductive services while preventing the formation of an embryo bank, no matter the size, further clarifying who should own embryos as well as the definition of embryo donation as it pertains to the current situation.
I don’t know about you but I don’t really like the idea of “McEmbryos,” or the commodification and “Wal-Martization” of human embryos. Patients should own them and decide their destiny. I am hopeful that our guiding societies will do just that – guide us on this sensitive and important topic.
Special thanks:
Thanks to Grace Centola, Ph.D., for helping to find the New York State statutes pertaining to embryo banking.
Thank you to Jessica Cussins for her blog on the topic, the reference by Professor Obasogie and her followup on the now closed Abraham Center for Life.
References:
Ethics Committee of the American Society for Reproductive Medicine. American Society for Reproductive Medicine: defining embryo donation. Fertil Steril. 2009 Dec;92(6):1818-9
.
24 Responses to “The Embryo Bank Dilemma: Reviewing the Issues, Historical Perspectives and Offering Potential Solutions”
Why Creating “McEmbryos” is Just Plain Wrong
Introduction
Recently, Alan Zarembo of the L.A. Times released a story alleging that California Conceptions was combining donated eggs with donated sperm and called them “donated embryos.” If there were leftover cryopreserved embryos, ownership of the embryos apparently went to California Cryobank (CC). If true, this is an egregious assault on reproductive ethics.
Defining embryo donation
About one-third of all patients undergoing in vitro fertilization (IVF) will have excess embryos to cryopreserve. About one-half of these will not be used for reproduction by the patients who created them. (Bangsboll et al., 2004; Lyerly et al., 2010) Embryo donation occurs when patients with unused cryopreserved embryos make the amazing decision to pay it forward and donate their embryos to patients in need. In true embryo donation, the patients own the embryos and make disposition decisions regarding their embryos. It is estimated that 2-10% of all cryopreserved embryos are donated to patients in need.
Why is creating “McEmbryos” so wrong?
Allegedly, California Conceptions would use donor sperm and donor eggs to create embryos. At times, all the resulting embryos would be transferred simultaneously to numerous couples, each receiving approximately two embryos at a time. This would commonly be called a “split donor/donor cycle.” It is, however, an absolute misrepresentation to call them donated embryos. At least in this split donor/donor cycle scenario, where all the embryos were transferred, there would be no cryopreserved embryos left whose ownership was uncertain.
What if not all the embryos were transferred and some were cryopreserved? As I understand, CC transferred no more than two embryos at a time to numerous patients, with the remainder cryopreserved. The residual cryopreserved embryos became the property of CC.

According to the article, egg and sperm donor profiles are sent to prospective recipients. As soon as CC received a “buy-in” from a few patients, the “donor embryos” were created from the donor eggs and sperm. Who made the decision to combine these two donors? What happens to the left over cryopreserved embryos? The article stated that dozens of embryos would be created through the combination of a pair of donors with the embryos then frozen while CC looked for patients who wanted them. And yet, the clinic claimed to have only ten sets of cryopreserved “donated embryos” in their tanks at any given time.
While they stated they didn’t want to create a bank, it would appear that this is precisely what was being done.
I feel there is a potential conflict of interest on the part of any IVF facility regarding the disposition decision of any cryopreserved embryos that they own. Patients normally have options such as using them to build their family, donation to science, donation to a laboratory for quality assurance testing and personnel training, keeping them cryopreserved forever, and finally, donating them to patients in need (embryo donation).
With the methods described in the article, a number of logistical and ethical questions arise:
- Were the sperm and egg donors fully aware of what was to be done with the resulting embryos?
- How did the IVF practice decide which sperm and egg donors should be combined? Was this decision made through market research? If so, who made these decisions?
- Is anyone tracking where all these donor-donor conceived offspring end up?
- Who ultimately owns the cryopreserved embryos? In the article, the physician interviewed said the clinic owned them when they were frozen
- Who makes the disposition decisions regarding these embryos? Will the IVF facility that owns the embryos be likely to make disposition decisions that do not benefit their bottom line? Who has the best interests of the cryopreserved embryos at heart when the embryos are owned by the IVF facility? Is it possible that CC is the entity that is really “donating” their remaining cryopreserved embryos
- What happens to the cryopreserved embryos if the practice closes or is sold?
- Perhaps most important, although it may not be a problem presently but for the future, what happens to the cryopreserved embryos that are never chosen?
While certainly not meaning to demean the cryopreserved embryos, I can’t help but think of these dono/donor cryopreserved embryos as fast food embryos or “McEmbryos.” I can just see the patients coming in, looking above the cash register to the menu above and ordering a “Number 3,” which has a burger (i.e., bright, blonde-haired, blue-eyed egg donor) and fries (i.e., handsome, athletic and tall sperm donor) and ends up getting the order supersized to boot (i.e., requesting twins). I should write clearly that this is not the current method CC uses to to match recipients to remaining cryopreserved embryos but the slippery slope exists and other practices may eventually emulate this process
What did EDI try to do over the past year to remedy the problem?
We suspected what might be happening at CC well over a year ago but didn’t have proof. We approached the American Society for Reproductive Medicine (ASRM) who examined the information and eventually sent it on to the Society for Assisted Reproductive Technologies (SART). SART did an investigation agreeing with our preliminary assessment. Unfortunately, CC was not a member of SART so they had little influence with CC.
There was some discussion of placing CC on the Center for Disease and Control’s (CDC) radar, asking that they potentially audit CC. I am not aware if this was ever done.
There was some discussion of revising the Ethic’s Committee Opinion on embryo donation detailing the inappropriateness of creating “McEmbryos,” but in the recent revision sent out to all ASRM members to review this past August contained no such language. I contacted ASRM and volunteered to help write the couple of paragraphs that would address the issue but I was never contacted. My current understanding is that the ASRM Ethics Committee will be taking up this issue in the beginning of 2013 and I am hopeful they will make a stand against creating “McEmbryos.”
Is it really ASRM or SART’s fault?
ASRM and SART are membership organizations. Anyone can join ASRM whereas SART is only open to IVF practices. These entities are not designed to truly police their members. Certainly, they can bar them from membership, but let’s face it, this is really not much of a punishment. Most patients are not really aware if a practice is a member of either organization, so expulsion does more to protect ASRM and SART from criticism than it does to protect the patients.
In reality, I am not suggesting that ASRM or SART begin sanctioning their members. These organizations are made up of bright individuals wanting what is best for members and patients alike. I don’t believe ASRM or SART could ever expose themselves to legal liability and try to be anything more than what they were originally designed to be.
I feel criticism towards ASRM and/or SART is potentially misplaced. While I do feel these organizations can certainly take a stand against the creation of “McEmbryos,” they can only provide educational materials and information to members and patients. never entering the realm of fining, condemning practices or policing practices. That is simply not their job.
I am not being insensitive to the needs of the patients
California Conceptions is providing amazingly healthy embryos to patients in need. How could anyone not be touched the story twin girls born to a single 41 year-old woman? There is no question that the donor/donor split cycle can be far more cost effective than many other options. The ends to this process are what we all strive for – a healthy family.
Call me old-fashioned but I still feel there are instances where the ends cannot justify the means. Are we are loosing all respect for the embryos and treating them utterly as a commodity? The slippery slope is becoming quite steep. Are we ready for expanding banks of unclaimed embryos across the country owned by practices or physicians and not the patients? I’m sorry but the means being used here are fraught with uncertainty and may result in a list of unintended consequences.
What are the potential repercussions of the L.A. Times story?

At least this election year is over. I had grave concerns that the story would break early in the election cycle and would become a political football, resulting in a series of consequences around the country. I still believe we are at risk in the following ways:
- • Poorly designed and reactive legislation may yet be created on state or national level
- • This story may motivate the “Personhood” advocates by encouraging them to win personhood for embryos thereby protect them from becoming “McEmbryos”
- • There will be “guilt by association,” leaving other legitimate embryo donation facilities open to criticism and ridicule
- • All of this will reflect poorly on basic IVF facilities that are frequently viewed as unregulated, even though we are accountable to more regulatory agencies than any other area of medicine
There may be significant backlash regarding this story and we should all be prepared to answer questions that may arise from the media, our peers and our patients.
How can embryo donation programs hold but not own the donated embryos?
At Embryo Donation International (EDI), the embryo donors are still able to request that their donated embryos be returned if needed. For example, if the children of an embryo donor were tragically killed in a motor vehicle accident, it seems absolutely appropriate that the cryopreserved donated embryos should be sent back to the donors. To discourage this from being done without good reason, transportation costs for returning the embryos, which is estimated to be $300, are the responsibility of the original donors.
Once the embryos are transferred into the recipients, however, they now “own” them. In this way, EDI never truly owns the donated embryos. We are the conservator and protect the embryos while never making any disposition decisions regarding their fate. We never own the donated embryos and we encourage all embryo donation facilities adopt this model of conservatorship.
What can be done to correct the current problem?
- Various membership organizations such as ARSM, Pacific Coast Fertility Society (PCFS), SART and RESOLVE could release position statements condemning the creation of “donated embryos” without a destination. This could help guide public opinion.
- Perhaps the embryo donation programs would be willing to sign a contract stating that they will not participate in the creation of embryos without a destination. Programs willing to sign and honor the contract would be adhering to the highest of ethical standards.
- Through the court of public opinion and if the L.A. Times article is accurate, patients may no longer want to participate in what they feel in an unethical practice.
- Legislative action on the part of California may be necessary but this will take time and a great deal of expertise. We run the risk, however, of having well-meaning legislative actions spilling over and harming the process of embryo donation or IVF itself.
- CC itself may need to modify its business model by allowing patients to own the cryopreserved embryos.
From my perspective, we have a few options:
Something really needs to be done. I don’t feel that this unethical practice should continue. A corporation, business or physician practice should never own embryos, no matter how brief. These embryos are also not truly donated unless you feel CC is able to donate the excess cryopreserved embryos. The question is if we should play an active or a passive roll in determining what takes place. I personally prefer the active roll so you can count EDI in on doing our best to guide the process.
Sour grapes? Nope, just sour taste!
CC is a potential competitor of EDI. I have made this clear to each and every person I have spoken to regarding this current dilemma. When we were contemplating the expansion of our ten-year embryo donation program into EDI, we also looked at the option of a money-back guarantee such as is offered by CC. Understanding the delivery rates for recipients of truly donated embryos ranges from 27-45%, the likelihood of returning the majority of the payments back to recipients made it unlikely we could even keep our doors open. Most “shared risk” options also charge a premium on top of the normal fees. Recalling that embryo recipients are emotionally and financially drained, the idea of tacking on a large additional fee seemed unfair to the recipients and quite impractical to the process. Embryo donation works for recipients, in part, because it is more cost-effective than many other options.
So you see, it is not “sour grapes” that is guiding my writing; it is just a sour taste. If the article was accurate, I feel strongly that creating “McEmbryos” is an affront to IVF and embryo donation programs, misleading to embryo recipients and totally unfair to the cryopreserved embryos that are currently waiting to be chosen.
If you agree, please co-sign this blog….
We are going to do something a bit different with this blog. We are strongly encouraging not just the routine comments that follow our blog but we are also asking that practices, patients and interested parties who agree that creating “McEmbryos” is ethically inappropriate sign below. By endorsing the statement below, we will hopefully begin to separate ourselves from such entities that practice the “McEmbryo” method of “embryo donation,” moving forward with a resolution that will work best for all.
routine comments that follow our blog but we are also asking that practices, patients and interested parties who agree that creating “McEmbryos” is ethically inappropriate sign below. By endorsing the statement below, we will hopefully begin to separate ourselves from such entities that practice the “McEmbryo” method of “embryo donation,” moving forward with a resolution that will work best for all.
By signing below, I do hereby agree that creating banks of cryopreserved embryos is ethically unjustifiable and support sound solutions that will adhere to the highest of ethical standards supporting patients and cryopreserved embryos in the best possible way.
References:
28 Responses to “Why Creating “McEmbryos” is Just Plain Wrong”
-
While I agree with you that using the term “embryo donation” for what is really a dual-donor shared cycle is misleading, I disagree that what CC is doing is inherently unethical. It is a slippery slope, yes, because there is potential for abuse in the system. CC offers hope to couples who are not eligible for what we normally think of as embryo donation. Face it, competition and waiting lists are scarce and many programs including yours are forced to discriminate, er, prioritize just because demand outpaces supply. Couples who need two donors but who cannot afford a traditional egg donor program have an opportunity with CC that they may not have anywhere else. I have a pair of friends who are pursuing conception through CC’s program now, and if this door also becomes closed to them they will be completely out of luck.
Unless you have reason to believe that CC is actually engaging in the potential unethical practices you mentioned – for example, dishonesty toward the donors or creating a bank of embryos that may never be selected by a recipient couple, I would ask that you not take away the one glimmer of hope some infertile couples have to grow their families. It may be reasonable to ask them to stop using the term “embryo donation” to describe their program, as use of that term is extremely confusing. But please don’t try to shut them down without very very good reason.
I myself have contacted CC as a potential client. We chose to go another route, as we had another option open up for us (I’m on your waiting list but I’ve been more or less assured I’ll never reach the top). I can assure you that the person I talked to at CC was up front about explaining their process to me and although their website is pretty vague I understood after talking to him that their program was a double-donor shared cycle. Even though we chose not to participate with CC’s program, I was the one who recommended it to my friend after she was turned down for an embryo donation program.
Please feel free to contact me if you would like to know more about my experience. I think my friend would also be willing to speak with you about her experience so far with them.
-
I’m choosing not to sign or leave my name, but I do agree with the above blog. My husband and I came very close to using CA conceptions to adopt embryos. We had the consult with Dr. Z, who was quite honest about what their process was. He explained that he would review our request, find 3 or 4 other couples who were looking for embryos with similar characteristics, then create a batch of embryos, splitting the batch among said couples for $9800 plus expenses. I kept asking Corey (the IVF coordinator) prior to my consult, who the original parents were. I could never get an answer from him. Dr Z. didn’t come right out and say it, but clearly there are NO original parents. I was able to persuade Dr. Z to send me a list of his egg donors, and that decided it for us. They had poor histories. Several had sexually transmitted diseases, a few had alcohol and drug issues, and I could not find a single donor without at least 6 or 7 piercings and/or tattoos. We opted for another, honest route, and I’m SO glad we did.
-
Dr. Sweet, the LA Times article is correct, though your perception of it is off on several accounts. I’d be happy to discuss this with you professionally, as you feel very compelled to bring this program to justice. Your points that embryos don’t have a destination, are sent to California Cryobank, and are somehow “designer babies” like a fast food order is entertaining, but far from accurate. Any embryos not being transferred are matched very quickly and really are no different than the embryos you are “holding”. Your own website has a call for people to donate their embryos to EDI. Does EDI own them without a destination? You could apply all of your same ethical questions from the moment the donating couple “donates” the embryos to you. Your only difference is a “take back” clause whereas we are matching the embryos with little to no delay.
All of your above questions are easy to answer and if you approach this fairly, I’m certain you’d be satisfied. Our recipients and donors are fully aware of the program and details. I am an ASRM member and would gladly answer their questions as well. We have been inspected by the FDA and the program was explained to them with no concerns raised. We had no deficiencies in our inspection and were commended on or organization. I have discussed the program with doctors from many respected IVF programs and most of them refer patients to us.
I would hope that out of the interest of fairness, you post my reply on your blog. I agree with your concerns that you have raised and would be happy to discuss your questions so you may be reassured California Conceptions is not “McEmbryos”.
Ernest Zeringue MD
California IVF Fertility Center
530-771-0177 -
Thank you Dr. Sweet for exposing this unethical practice.
-
Thank you for posting my comments and responding. While you did not use the term “designer babies”, it was fully implied by your paragraph about ordering a “Number 3”. The blog did not discuss other programs, it direcectly implicated my program of unethical practices. We don’t know eachother personally so I’m not taking it that way at all. I think it’s important to not have the program accused of things that simply aren’t true.
Beacuse there are always possible “slippery slopes”, this should not preclude ethical fertility practices from helping patients. With the proliferation of IVF itself, many people proclaimed it wrong because of potential ethical abuse. The field will continue to evolve and we should continue navigating our way to providing patients with options for preganancy. We agree on this point so it comes down to how we go about doing this.
Our programs are different and can not be directly compared on all levels. My program is not by default wrong because it doesn’t follow your model of handling embryos. The mear designation of “ownership” to a large extent is irrelevant. What are we doing with left over embryos? Matching them to another couple. Are we deciding thier disposition? Yes, we are matching them to another couple. Are there scenarios of ethical abuse? No, saving freezing them after a fresh cycle and matching them to another couple (usually before the cycle starts or within a week) is not the same as an embryo warehouse or cryo bank in the sense of sperm or egg banks. The disposition of embryos is pre-determined as part of the program and we are not deciding anything other than matching. Embryos are treated as “potential people” and the opportunity for a couple to have a child. We both value this potential obviously. There is no alternative for the embryos other than transfer and no benefit to anyone to treat them otherwise. Establishing “ownership” really has no part in this process. We don’t “own” our children thoug we are responsible for them. Embryos aren’t given status as a person, so does that by default mean we have to “own” them? Does “owning” them mean we can do as we please? If you really dig into this arguement you can quickly see how it can become irrelevant. A transient period from cryopreservation to a subsequent match does not constitute a “bank”. We both agree that a bank of embryos like a sperm bank or egg bank is not what we are after. Yes there is a slippery slope and others may go down an undesired path, but until we do, we have not created a true bank. We may not agree on this but that by defualt does not make us wrong or unethical. Are there examples where we have done anything that is unethical with the embryos?
The comment about 10 sets embryos in cryopreservation referred to 10 sets that were cryopreserved and not already mached. It’s uncommon there are even that many because of the logistics of how we match – I had to come up with a number during the interview and estimated 10 sets. Matching is very fluid and dynamic so the number changes as people make selections and new donors go through the program. There may be times that we have embryos frozen that have been accepted and are scheduled for transfer, but in my mind these now “belong” to the recipient. Outside of sending you our inventory logs, there is no real way to prove this. I stand by my original statement as it pertains to unmatched sets.
Recipients are free to select profiles or pass and wait for additional matches – similar to other programs with donated embryos. We are not forcing them to select anything and are not making decisions for the recipeint. The donors’ profiles are available to the recipients as you can tell by the post above. Again, this may not match your program, but I don’t believe any one program establishes the standard.
Feel free to email or call. If I’m tracking things right, it seems your only real concern with California Conceptions at this point is the “banking” phase. We may not agree on the terms banking and ownership as it applies to California Conceptions, but I think we both agree that we don’t want to see embryos banked in a similar manner as eggs and sperm with large catalogs and a supply that exceeds the demand (yes, I cringe at these terms too).
Ernest Zeringue MD
California IVF Fertility Center -
[…] Dr. Craig Sweet of Sweet Fertility published a thought-provoking blog post entitled “Why Creating McEmbryos is Plain Wrong” which describes his misgivings with the alleged practices of another infertility clinic, […]
-
Thanks Dr. Sweet for posting this question. I agree that we need to consider all the ramifications of these evolving services. My personal experience with in-house embryo donation among patients in a fertility clinic makes me think that temporary custodial “ownership” if you will of embryos by clinics is probably a more common thing than you might think during the matching process. I see obvious advantages to patients from the CC approach–the ethics of any of this is determined by the details of how it is handled by each program. The real unanswered question for me is regarding the resulting children. Have we created systems that allow these donor -conceived children to have the option of finding their biological roots- either their siblings or possibly- if both parties agree–their biological donors? In our rush to satisfy the needs of our patients, are we paying too little attention to the effect of our services on their children? Or is that simply not our problem as providers? I don’t have the answers but I certainly welcome the discussion. I posted on the “embryo creation for donation” topic on my own blog. http://bit.ly/SmkZIV
-
I disagree that what CC does could be considered unethical. My main purpose in commenting, however, is not to attempt to add to their excellent defense…but simply to say there’s nothing wrong with requesting, if possible, an embryo who approximately matches the parents-to-be and their characteristics… my husband is Filipino and I am Caucasian, and to wait for a naturally donated embryo to match this racial mix would take forever. I find it much more troubling that their egg donors may be unhealthy individuals…but that’s an issue any recipient has to investigate for themselves, regardless of the program.
-
On this point, I agree with you Dr. Sweet. When I heard about the services that California Conceptions offers, I couldn’t help but cringe at the thought of embryos being created via complete strangers. That in and of itself is a slippery slope indeed. As I’m sure you’re aware, I’m more concerned for the pre-born humans that will have to deal with that reality in adolescence and adulthood. While a minority will not struggle at all with their creation, I have not doubt that quite a few will. Questions like: What are my origins? What are my roots? Why did my genetic parents choose to donate? Did they think about how this might affect me in the future? Do I have full genetic siblings in this world? Can I have access to my medical history? Who am I?
It’s way too easy to create pre-born children that literally have no voice in the early years. Do we just shrug our shoulders and wash our hands of how this might affect them when they do form an opinion about those responsible for the way in which they were created? Do we have a responsibility to create ethical standards that will span the years, knowing the decisions we make now WILL affect a human being well into the future? Or should those children just keep their mouths shut and be grateful that they were created at all?
Something to ponder.
-
I have POF and my husband has sertoli cell only syndrome so in order for us to have a pregnancy and a child we would have to do a double donor cycle. This is exactly what I am doing at CC. I can also do that at Shady Grove, or my local fertility clinic but the difference is, I would be paying at least $20,000. Splitting the cycle makes it affordable. Why is there scrutiny on CC but not on other clinics that offer split egg donor cycles? Singling out CC seems like the work of those that feel CC has an unfair advantage. Because they’re offering a service at an affordable price they are being targeted.
-
Dr Sweet I agree with you that the utmost care should be taken to ensure that embryos are handled in an ethical manner but I fail to see how California Conceptions has handled the embryos in a way detrimental to those said embryos. As I understand it you have two issues with the California Conceptions business model, one, that they own the embryos and that ownership “could” be a slippery slope for some other businesses to create an unethical business practice and bank dozens and dozens of embryos. And two, that they are calling the embryos “donated embryos.”
If California Conceptions has not been shown to have done anything unethical I think it’s completely unfair to call their practices unethical based on what other businesses might do in the future. They are not sliding down that slope and should not be held responsible for what other businesses might do in the future.
As far as calling the embryos “donor embryos”, the embryos are created from donor egg and donor sperm and in my mind it is not wrong or unethical to call them donor embryos. I agree with you that your definition of donor embryos is different but that does not make California Conceptions wrong, just different. I would be interested to know what you think they should be called? I am a current patient of California Conceptions and am now five weeks pregnant through their program. I cannot say enough good things about my experience with CC. I was made very aware that the embryos were from a shared donor/donor cycle when I first contacted the clinic. As it turned out the embryos we were planning to transfer from a fresh cycle did not progress as hoped. We were provided with an alternative profile, previously frozen from a fresh cycle a short time earlier. I have no issue with my unborn child/children having at one time been called a donor embryo. I am however deeply offended by having my unborn child called a “McEmbryo.” We only asked CC to match us with embryos “similar to us.” We did NOT order out of a catalog a designer baby.
I would also like to address the comments made earlier in this blog regarding the health of the donors. We were provided with extensive medical background information for both our prospective fresh cycle and the alternative frozen profile donors. None of the donors in those profiles had any medical issues in their histories, which as I said was extensive and included their family histories. I do not consider tattoos or piercings medical red flags but neither of the egg donors had “6 or 7” and neither of them had had any sexually transmitted diseases. Also, like Dr Z stated we were given the profiles with the opportunity to approve or disapprove the match if there had been any issues.
Lastly, I have given a great deal of thought to what we will tell our little one when they have questions and it will never be secret. Our child will always know how much they were wanted and loved. We believe the donors are to be appreciated for the gift they have given so we can have a child in our life that we so desperately wanted.
-
One more comment Dr. Sweet. There are many, many Fertility clinics around the U.S. which have donor embryo programs. Most of these are anonymous donations from previous patients. The embryos are donated to the clinic. The clinic does paperwork to transfer ownership of the embryos from the genetic (or original parents…sometimes these embryos were created using donor material) to the clinic. They are then “owned” by the clinic until a suitable match is made to a donor couple. This is usually a short time, but not always (sometimes the embryos are not of great quality and are rejected by recipients). Will you now be going after all of these clinics as well…stating they are unethical and creating embryo banks? When you take a stand on a subject like this publicly, keep in mind you may end up harming the practice in general. This is another reason I would caution you about posting public opinions on an “article” you read before contacting the subject (Dr. Z) directly and discussing it with him. It just seems like if you have a beef with someone….talk to that person before slinging around derogatory statments like “McEmbryos” and “A number 3” regarding their practice. Other than a short window of time where minimal embryos are cryopreserved….Cal Conceptions has debunked all of your “concerns” about the creation of the embryos without intended parents…they are not shipped off to Cal Cyrobank for eternity and the recipients don’t provide a long list of designer details they want in their embryos. Most people just want a healthy baby with an ethnic/race similar to their own. When I went through the traditional program….we had ZERO requests on race/color/creed…we just wanted a healthy baby. I know several couples who have gone through donor cycles (personally, through blogs and on forums)…the vast majority have very few requirements other than good health and a close ethnic match. Of those who do make extensive lists…they wait longer or end up not doing it because most programs won’t cater to those minute details.
Just more food for thought here.Regards,
KD -
As a hopeful future patient of California Conceptions, I fail to see the ethical concerns that you have regarding this program.
In a traditional IVF cycle, a dozen or more embryos may be created with the intent of using only 1 or 2. The remainder may be donated to other couples, but in reality, most are either destroyed or frozen indefinitely. Many embryos are created with the intention that only a few will ever be given the chance at a life.
My understanding of the CC program is that every healthy embryo will be implanted into a women and given the chance to develop into a baby that will be loved and cherished my parent(s) who desperately want a child. Most embryos have “intended parents” before they are even created and the ones that are frozen only remain so for a short time until they are matched with parent(s). This seems like a better ethical approach to me since all embryos created will actually be given a chance at life as opposed to being frozen for all eternity.
Quibbling over who does or does not “own” the embryos seems nonsensical when the most important consideration should be what percent of these created embryos will ever be given a chance to become human beings. I think CC wins hands down in that regard!
-
I find it very interesting that you took the time to blog about your opinion of a clinics practices without ever contacting the clinic to gain any firsthand knowledge. When I google your clinic some less than complimentary reviews come up from previous patients. Should I base my opinion of you and your practice on that?
My husband and I tried for years to get pregnant using donor sperm with no success. When we decided to add donor eggs to the mix we knew we only wanted one (two only in the case of twins) child. If we went to a traditional egg donor we would have to decide what to do with the remaining embryos and we didnt want to be faced with that. We chose CC and haven’t looked back.
For you to pass judgement on a clinic without finding out for yourself what’s really going on there is misleading and inappropriate.
Our child(ren) will know exactly where they came from which will illustrate to them how badly they were wanted. Unfortunately now one day they are going to google CC and find the judgemental uninformed opinions of one of their competitors, a supposed expert in the field, and have to second guess their origins. Thanks for that. -
I know that well-meaning people can have vastly different perspectives and therefore different opinions on ethical issues that arise with ART. I am grateful that Dr. Sweet is bringing up controversial topics–apparently hitting some nerves–but I think we need to continue to ask these and future questions. I think that we owe patients continued thoughtfulness about how we do ART. To this end, we should continue to have more transparency about the nuts and bolts of how we offer ART services in this relatively unregulated medical environment. Let’s make sure to encourage continual self-examination of our services and not shout down those that ask the hard questions within the field. Best Wishes.
LinkedIn Groups for Medical Professionals and Support Staff Who Share a Common Interest
Time is simply too scarce!
I will be the first to say that I don’t have enough time. Not enough time to work and certainly not enough time to play. With the advent of social media, I found my time even more precious. It is not that I spend my time socializing on these social networks. I am using it to communicate better with my patients and my peers. Unfortunately, each piece of the time pie just keeps getting cut smaller with the smallest segment seemingly used for sleep.
Why not Facebook and Twitter?
Now, I will be honest with you. I am also uncertain if there is true value with my being on Facebook and  Twitter. Yes, I try to post interesting information for my patients and peers and tweet witty phrases for all that actually follow what I might say. But I can’t help but feel that everyone, including myself, is overwhelmed with the vast sea of distractions that follow us on our computers, phones and iPads, 24/7 and wherever we go.
Twitter. Yes, I try to post interesting information for my patients and peers and tweet witty phrases for all that actually follow what I might say. But I can’t help but feel that everyone, including myself, is overwhelmed with the vast sea of distractions that follow us on our computers, phones and iPads, 24/7 and wherever we go.
What were the alternatives?
Let me digress for a discussion on what I did when a difficult issue cropped up in my world of embryo donation. I could certainly talk to my staff, e-mail my connections or actually use the old-fashioned phone to toss the dilemma around with my peers, but connecting wasn’t at all easy. It is hard to catch people at the right time and plus I couldn’t get more than one or two opinions over a few days.
E-mail list services (commonly called “listserv”) are interesting entities, reminding me of on-line bulletin board of days gone by but significantly more difficult to follow. While listservs are really useful to target a group of people with similar backgrounds, it wasn’t necessarily the best way to reach people of varying experiences and professionals in different fields that might have a perspective to add. Don’t get me started on how difficult they can be to read as many simply click reply re-copying all that was on the e-mail to start. When a number of people do this over a short period of time, the e-mail gets very long and very difficult to decipher important information from the din of republished material. They are probably the second best option but they simply are not that easy to work with.
Why LinkedIn?
 So, please understand that I was skeptical when I began to play with LinkedIn. Setting up my profile wasn’t complex but I wondered how useful it would be compared to my more comprehensive C.V. The problem was that patients and peers had to search for my C.V. whereas LinkedIn was providing the basics with the click of a mouse. OK, that was a plus but what about the rest of LinkedIn?
So, please understand that I was skeptical when I began to play with LinkedIn. Setting up my profile wasn’t complex but I wondered how useful it would be compared to my more comprehensive C.V. The problem was that patients and peers had to search for my C.V. whereas LinkedIn was providing the basics with the click of a mouse. OK, that was a plus but what about the rest of LinkedIn?
I knew that LinkedIn was described as the “Facebook for business” but I couldn’t really see my peers trolling LinkedIn as some are glued to Facebook. Certainly, if you are looking for an employee or for a job, it might be a great place to start, but what was the use of making all those connections when I wasn’t really doing anything with them? Did I really need to enter a popularity contest and see how many connections I could make? Really, not my style.
Why LinkedIn Groups?
Deciding I needed to create a social media forum where I might be able to coax others interested in the professional aspects of embryo donation to join me, I turned to LinkedIn Groups. LinkedIn Groups seemed to be ideal with it’s easy to read and understand format. I created the Embryo Donation Network.
There are strengths with LinkedIn Groups
My intention with the group was akin to the goal of large national/international infertility meetings where all types of professionals with similar interests converge, but to do this within the comfort of the professionals’ home or offices.
- I am able to screen the members, keeping only professionals in the group and politely redirecting patients to a host of other online information.
- I can utilize the many links I have created over the months, asking reproductive endocrinologists, reproductive attorneys, medical ethicists, embryologists, IVF coordinators, mental health professionals and administrative support staff who might have a potential interest in embryo donation to join the group.
- Polls are quick and easy, much easier that Constant Contact or even MailChimp from my perspective.
- I can control posts if desired or simply let the members direct the conversations, posing tough questions that we need each other to help figure out.
There still are some weaknesses with LinkedIn Groups
While I am still learning how to use the LinkedIn Group, there seems to be some sticking points that I haven’t quite figured out how to completely remedy.
- I can’t underline or bold words or sentences or easily add photos when I think greater emphasis is needed.
- It is not always easy to get the conversations started. I sometimes have to post a question a second time for someone other than myself to continue the conversation.
- It is too easy for the same talking heads to lead the group, and that certainly includes myself! Motivating other members is a challenge.
- While balancing the need for a continuous conversation without overwhelming the members, unless you have an active moderator, most groups seem to die a slow death.
- Unless I am missing something, I can’t seem to close and archive some conversations that I feel should be shelved for now.
- Some of the groups are just pure self-promotion. I’ve made it clear that posts such as these will have to be tossed into the Job section, the Promotion section or simply be removed. I think this is the biggest turnoff to the LinkedIn groups these days.
My eventual wish list for LinkedIn
Perhaps someone from LinkedIn will actually read this blog and consider the weaknesses listed above and the wish list I created below:
- If someone joins my group, it should be easier for me to add them to my network. As it stands, I have to know their e-mail address to connect to them and I don’t have this on many of my group members.
- It would be truly wonderful to have a bunch of live talking heads discussing issues though live audio and perhaps video feeds. Creating such a meeting place would be invaluable.
- Some sort of detailed analytics report would be useful for trying to see what topics created the greatest level of discussion. One has to track this by hand to see the patterns and Google Analytics does this with more ease for websites.
The Embryo Donation Network is the best method I have found to communicate with professionals who have a similar interest
Where else could we get some amazingly accomplished people into embryo donation conversations? Where  else can you get so many professionals to pay close attention to a single topic for any length of time? Since launching early this year, we now have approximately 180 members and continue to grow. Compared to the LinkedIn groups for RESOLVE that has 843 members and ASRM that has 516, I think we are doing just fine. And it is not really about numbers, it is about the quality of the discussions among experienced professionals.
else can you get so many professionals to pay close attention to a single topic for any length of time? Since launching early this year, we now have approximately 180 members and continue to grow. Compared to the LinkedIn groups for RESOLVE that has 843 members and ASRM that has 516, I think we are doing just fine. And it is not really about numbers, it is about the quality of the discussions among experienced professionals.
So, if you are a professional interested in embryo donation, especially its ethical, medical, psychological and legal aspects, then the Embryo Donation Network is for you. Please join LinkedIn, change your search category (found in the upper right corner of your LinkedIn home page) to “groups” and type in “embryo donation” to find the Embryo Donation Network. From there, simply click, request to join the group and you will be added quickly. I promise not to overwhelm the members; my intent is to post only one general topic per week. The only perquisite is that you are truly interested and, hopefully, somewhat willing to jump right into the fray and interact with other professionals who share your interest.
Do I miss posting as many messages on Facebook for my patients and peers? Not really, as I am not naturally a social animal. I’d rather read an article than discover someone liked my last post or if we have created any new connections. Have my number of tweets decreased on Twitter? You bet. Have the number of articles I commented upon in Digg fallen? Certainly. Am I sleeping a bit less? Inevitably so. But what has vastly improved is my ability to reach out to some highly skilled professionals and pick their brain when mine is a bit confused. I also hope that I may, in some small way, be teaching others about the amazing world of embryo donation one topic at a time. Come and join the fun – join LinkedIn’s Embryo Donation Network!

Craig R. Sweet, M.D
Reproductive Endocrinologist
Practice and Medical Director
Embryo Donation International
And more importantly….
Moderator, Embryo Donation Network
2 Responses to “LinkedIn Groups for Medical Professionals and Support Staff Who Share a Common Interest”
-
Certainly the most active group w/which I am engaged. What’s really cool is the various perspectives being shared by other pros working in assisted family building, I don’t agree with everything that has been posted but I do enjoy and value the opptny for connection and exchange w/colleagues.
What Impacts Embryo Donation Success Rates?

Craig R. Sweet, M.D.
Reproductive Endocrinologist

Corey Burke, B.S., C.L.S.
Laboratory Supervisor
Introduction
Asking what determines the success rates in embryo donation is an excellent question. The answer, as one might expect, is neither simple nor completely understood.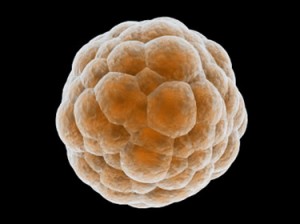
Embryologists and physicians try to choose the fewest number of healthy embryos for fresh transfers to increase success rates while minimizing multiple pregnancy rates. It is indeed a delicate balance. For example, it is well understood that in Europe, physicians transfer fewer embryos but patients also suffer significantly lower success rates than in North America. (Boostanfar R, et al. Fertil Steril 2012)
What variables do we examine to estimate probable success?
Since donated embryos are cryopreserved, the variables become even more complex compared to fresh embryos. In combining a great deal of published data and over 20 years of IVF and embryo transfer experience, we came up with what we feel are the variables which seem to influence success rates:
| Very Important! |
Preferred |
Less Optimal |
| Did the fresh cycle in which the embryos were frozen result in a pregnancy & delivery? |
Successful pregnancy and delivery |
Fresh transfer resulted in miscarriage or no pregnancy |
| Number of embryos available in a given donated set |
Four or more |
Three or fewer |
| Past implantation rates of both fresh and frozen embryo transfers |
High implantation rates |
Low implantation rates |
| Quality of the embryos frozen (link) |
High quality (Blastocyst) |
Medium quality |
| Age of the women when the eggs were provided to create embryos |
Less than 35 years old |
35 years of age or older |
| Overall health of the embryo recipient (link) |
Healthy |
With treated or untreated medical issues |
| Important |
Preferred |
Less Optimal |
| Stage of growth when the embryos were frozen (link) |
Day 5, blastocyst stage |
Day 3, 8-cell stage |
| Technique used to freeze/thaw or vitrify/warm the embryos (link) |
Vitrification |
Slow freeze |
| Overall frozen embryo transfer pregnancy rates for facility freezing the embryos |
30% or more |
Less than 30% |
| Overall frozen embryo transfer pregnancy rates for facility thawing the embryos (EDI) |
High at 30% or more |
Less than 30% |
| Ejaculated vs. surgically aspirated sperm used for fertilization |
Ejaculated sperm |
Surgically aspiration sperm |
| Somewhat Important |
Preferred |
Less Optimal |
| Was preimplantation genetic testing of the embryos done? |
Yes |
No |
| Age of the male producing the sperm |
Less than 40 years old |
More than 40 years old |
| Past successful deliveries with other embryos from donating facility |
Yes, with past deliveries |
Miscarriage, reduced survival of embryos or failed implantation |
| Probably Unimportant |
Preferred? |
Less Optimal? |
| Cryopreservation duration |
Less than 10 years? |
More than 10 years? |
The above variables influence EDI’s decision to both accept embryos from other facilities as well as determine how many donated embryos should be thawed/warmed to achieve a successful delivery.
The importance of the embryo recipient’s health should not be underestimated
In a previous blog, we described how important it was for our embryo recipients to be healthy. (link) Inadequately treated health problems, harmful medications, recreational drug use as well as smoking and weight concerns all play a potential role affecting success rates. It is clear that success depends on both the quality of the donated embryos and the overall health of the recipient.
Are all donating IVF facilities the same?
We understand that not all IVF facilities have the same success rates. Some facilities will have provided EDI  donated embryos with consistently high implantation rates while others may provide embryos of consistently lessor quality. EDI examines a facility’s past fresh and frozen embryo transfer pregnancy rates as well as its past history of providing EDI with donated embryos. It does, however, take a fair amount of time to seemingly identify a trend but we endeavor to examine all the variables we can. Our contact management database system was recently upgraded to track these variables more consistently.
donated embryos with consistently high implantation rates while others may provide embryos of consistently lessor quality. EDI examines a facility’s past fresh and frozen embryo transfer pregnancy rates as well as its past history of providing EDI with donated embryos. It does, however, take a fair amount of time to seemingly identify a trend but we endeavor to examine all the variables we can. Our contact management database system was recently upgraded to track these variables more consistently.
Do your embryos make the grade?
Understanding that all of the above variables are quite complex, we endeavored to find a simple way to convert the data into something patients could more easily understand. Since nearly all patients understand the basic A, B & C grades we used to receive in school, we modeled our grading of the embryos around these letter grades.
We created a mathematical model to assess a number of the above variables, converting the final analysis to A+, A, A-, B+, B and B- letter grades. Interestingly, we found the model really did help to predict delivery rates and continue to use it to this day to grade individual embryos as well as entire sets of donated embryos.
What information do we gain on the day of thaw and embryo transfer?
Most frequently, the embryos are thawed just hours before transfer. At times, we may thaw them days prior if, for example, they were frozen early in their development and we want to grow them further before deciding how many to transfer. Therefore, the following last set of variables will also influence success rates:
| Important |
Preferred |
Less Optimal |
| Survival rates of thawed embryos |
100% |
Less than 100% |
| Overall appearance of the thawed embryos |
Healthy, expanding and growing |
Evidence of cellular damage |
If 100% of the embryos, perhaps three out of three, survive the thaw and look healthy, we feel this is a good sign. If only 50% survive, for example perhaps only two of four, then we are concerned that the overall implantation rates will be reduced and that we might need to find more embryos to transfer just to get to the “finish line” of pregnancy and delivery. Ultimately, we want at least two high-quality embryos or up to four less certain quality embryos placed on the day of transfer.
What are the national success frozen embryo transfer delivery rates?
 In 2009, the CDC reported that there were 26,069 frozen embryo transfers performed in the U.S. with an average delivery rate of 31% per embryo transfer procedure. In addition, there were 6,074 frozen embryo transfers using embryos created from donated eggs (i.e., younger women) with slightly higher delivery rates of 34%. Please recall that donated embryos generally come from the very same types of patients listed in these success rates.
In 2009, the CDC reported that there were 26,069 frozen embryo transfers performed in the U.S. with an average delivery rate of 31% per embryo transfer procedure. In addition, there were 6,074 frozen embryo transfers using embryos created from donated eggs (i.e., younger women) with slightly higher delivery rates of 34%. Please recall that donated embryos generally come from the very same types of patients listed in these success rates.
What are EDI’s success rates?
We do our best to screen the embryos, carefully trying to choose the embryos most likely to implant. We estimate delivery rates with donated embryos to range from 27 – 42%, depending on the many variables listed in this blog, with a multiple pregnancy rates of 20-25%. We wish the success rates were higher, but please understand that frozen/thawed embryos implant and grow less frequently than fresh embryos and these percentages are entirely consistent with the frozen embryo transfer success rates described in 2009, which ranged from 31-34%.
Even with the slightly lower delivery rates compared to fresh embryo transfers, embryo donation remains one of the best and most cost-effective options for patients who cannot otherwise afford egg donation or qualify for adoption. Embryo donation still allows a woman to experience pregnancy and delivery while bonding, nurturing and protecting the ongoing gestation.
Summary
There are many variables that go into determining the potential success rates for a given set of donated embryos. First, we attempt to examine these variables carefully in deciding if EDI will accept the donated embryos. Second, we use this same information to determine how many embryos we should thaw/warm and eventually transfer. The process remains a bit of an ART (pun intended) since the complete understanding of how all of these variables influence each other and the ultimate success rates are yet to be fully known.
References
“Annual ART Success Rates.” Centers for Disease Control and Prevention. Division of Reproductive Health, 19 Apr. 2012. Web. 24 Apr. 2012. <http://www.cdc.gov/art/ARTReports.htm>.
Boostanfar R, Mannaerts B, Pang S, Fernandez-Sanchez M, Witjes H, Devroey P; Engage Investigators. A comparison of live birth rates and cumulative ongoing pregnancy rates between Europe and North America after ovarian stimulation with corifollitropin alfa or recombinant follicle-stimulating hormone. Fertil Steril. 2012 Mar 27.
3 Responses to “What Impacts Embryo Donation Success Rates?”
-
I am hoping to become pregnant with either embreo adoption or egg donation.
Can I pumyself on the list for embreo adoption? -
[…] found a very good blog post called “What impacts Embryo Donation Success Rates?” which does a very good job of explaining the criteria that embryo donation centers look for […]
Reasons to Donate
By: Vicki D., an embryo donor
“In the order of nature we cannot render benefits to those from whom we receive them, or only seldom. But the benefit we receive must be rendered again, line for line, deed for deed, cent for cent, to somebody.’ – Ralph Waldo Emerson, Compensation
On May 13, 2010, I made a decision. It wasn’t your normal everyday decision on things like what shoes to wear, where to have lunch, or which shade of lipstick to buy. It even surpassed those important decisions we encounter in life such as what house to buy, the most lucrative financial investments and selecting the best care for elderly parents. It was a decision much more substantial, incredibly emotional and most importantly, everlasting. It was regarding the fate of our embryos. Yes; five embryos, frozen, suspended in time – a significant and extraordinary reminder of a successful IVF cycle producing twin girls just two years prior. Considering that my family was now complete, the desire to have more children had abated. But the process was far from over and I knew this going in. There are five potential lives to consider currently residing in a sub-zero environment. So the question remained… what did one do with extra embryos when one’s need or desire to expand your family has subsided?
In my quest to determine the future of my five frozen embryos, I discovered several options to choose from. These ranged from permanent storage – or in some cases “abandonment,” destruction, donation to stem-cell research,  donation to the IVF clinic lab, or donation to an infertile couple or person in need. Continued voluntary storage brought unnecessary substantial fees, not to mention the inevitable procrastination of decision making. Abandonment wasn’t an option for obvious reasons as I felt a responsibility towards these embryos. The only things I have ever abandoned in my life were the occasional art project or my first premature marriage in my early twenties. The concept of destruction simply didn’t make logical sense. Why go through all the expense and trouble of creating embryos that one day would be destroyed because there was no better option considered? Stem-cell research or IVF clinic donation seemed like fair choices since I wouldn’t have my twins without past research in IVF. Even so, there had to be a better option available that would help promote the preservation of life and help out infertile couples desperately wanting a baby.
donation to the IVF clinic lab, or donation to an infertile couple or person in need. Continued voluntary storage brought unnecessary substantial fees, not to mention the inevitable procrastination of decision making. Abandonment wasn’t an option for obvious reasons as I felt a responsibility towards these embryos. The only things I have ever abandoned in my life were the occasional art project or my first premature marriage in my early twenties. The concept of destruction simply didn’t make logical sense. Why go through all the expense and trouble of creating embryos that one day would be destroyed because there was no better option considered? Stem-cell research or IVF clinic donation seemed like fair choices since I wouldn’t have my twins without past research in IVF. Even so, there had to be a better option available that would help promote the preservation of life and help out infertile couples desperately wanting a baby.
I remember the years of anguish I experienced being infertile. Everywhere I went I saw pregnant women or newborn babies. It became an obsession, perceived as something so intangible for me yet came so easily for others. There would be no remedy but a child. Why not help another couple expand their family? Why not help end the anguish? Why not “Pay it Forward” to the infertile community in such desperate need? The simplest answers to these questions became the best option.
So the decision came with three stages. Firstly, there was the genetic hurdle to consider. There is something about setting your genetic code, or more specifically, your potential genetic offspring, free into the world that can be somewhat unsettling. Where will these embryos end up, will they survive and what kind of life will they have? Will they know their history? Will they have questions? Will they look like me? But in the greater scheme of things, do these questions really matter?
The value and definition of family transcends any DNA makeup.
In the pursuit of the family unit, we tend to look beyond the genetic code and focus on the family element. The concept of having a family does not automatically equate to comparable genetic material as can be seen with any family with an adopted child. It’s about being part of a team, functioning as a whole and sharing your love and commitment to live and experience life together.
Secondly, there is an element of giving back; Paying it Forward to the infertile world. Donating the embryos was my way of paying back what I was so very fortunate to finally have – a family. Prominent memories of being unfulfilled without children are still fresh in my mind. I honestly believe that donating my idle embryos to someone in need helps to promote the probability of life.
And finally, chance. The chance to help someone build a family, the chance of potential life for the embryo, the  chance for you to give the greatest gift in life, the chance to take a chance! So for any of you out there who find yourselves with important decisions to make about your embryos in storage, think back a bit to your own infertile days. That memory will help guide you to do the right thing for someone with the same needs and desires as you have. Take a chance and do something good for humanity.
chance for you to give the greatest gift in life, the chance to take a chance! So for any of you out there who find yourselves with important decisions to make about your embryos in storage, think back a bit to your own infertile days. That memory will help guide you to do the right thing for someone with the same needs and desires as you have. Take a chance and do something good for humanity.
Donating the embryos was my way of paying back what I was so very fortunate to finally have – a family.
In the end I trusted Embryo Donation International (EDI) and Dr. Sweet with my precious embryos. I knew that with their high ethical standards and sheer devotion to the embryo they would give my embryos a chance at life, and hopefully help to build another family, just like they helped to build mine. And on every Mother’s Day ever since the donation I hope and wonder that by liberating my embryos they were able to help create another family somewhere out there and that they are as happy as I am.
Vicki D.
Mom, a Loving Wife and now, an Embryo Donor
torig71@gmail.com
Federal Funding of Embryo Donation and “Embryo Adoption:” Is it time for the Federal Government to Reconsider Its goals?

By: Craig R. Sweet, M.D.
Reproductive Endocrinologist
Info@EmbryoDonation.com
The “Defunding” of a Government-Supported Program
On March 2, 2012, it was reported that the Obama Administration wanted to defund the embryo donation/adoption awareness federal program that has been run by the Office of Population Affairs, part of  the U.S. Department of Health and Human Services. Spokespeople from Nightlight Christian Adoptions, the National Embryo Donation Center and Snowflakes Embryo Adoption programs were quoted as opposing the defunding decision. It should be noted they all had received or were receiving funding from the federal program, so their reactions were not unexpected.
the U.S. Department of Health and Human Services. Spokespeople from Nightlight Christian Adoptions, the National Embryo Donation Center and Snowflakes Embryo Adoption programs were quoted as opposing the defunding decision. It should be noted they all had received or were receiving funding from the federal program, so their reactions were not unexpected.
Initially, the federal program was created in response to President Bush’s push to use cryopreserved embryos to create families and steer away donations from human embryonic stem cell research. Since 2002, over 22 million dollars has been spent by the federal government on the awareness programs.
The Predictable Response
Certainly during an election year, the firestorm that followed was probably predictable.
There were calls stating that the Obama Administration was “pro-abortion,”
I’ve never met such a person in my entire life, although many have been “pro-choice.”
Congressman Chris Smith, a New Jersey Republican, was quoted a saying, “Assertions that leftover embryos are better off dead so that their stem cells can be derived is dehumanizing and cheapens human life.”
Come on now… this decision does not mean that all cryopreserved will be destroyed. It simply means that all of us who are dedicated to the concept of embryo donation need to work harder and smarter with non-federal funds to make certain patients are aware of the embryo donation option.
Mailee Smith, staff counsel at the “pro-life” Americans United for Life, was quoted, “What we’re seeing is the elimination of the moral solution.”
Nothing could be further from the truth. Many programs throughout the country offer embryo donation and will continue to do so long after federal funding disappears.
Could we all just trim the hyperbole a bit?
Is it a Coincidence that the Phrase “Embryo Adoption” Predated the Personhood Amendments?
I suggest paying less attention to the hype and instead examine the realities of the ways that federal funding can influence the competitive free market with unintended consequences. The propagation of the term “embryo adoption” sprouted the appearance of the personhood amendments and legislation, which are focused on declaring that eight-cell early embryos are people. The consequences of these enactments are far reaching, including monumental legislative changes, restrictions on the care of women, and severe restrictions to the treatment of the infertile patient. (See my previous blog on the Mississippi Amendment here.)
Not Sour Grapes but Concerns Regarding Discrimination
Let it be understood that Embryo Donation International (EDI) applied last year for the federal funding in question, but we were not awarded a grant. In partnership with professors at Florida Gulf Coast University, we proposed thirteen different fresh and innovative projects to increase awareness, as well as provide embryo donation services. While we were disappointed, we were not surprised that the organizations, for the most part, receiving funding had been granted it before and this was our first submission. EDI was not previously dependent on the funding so there were no significant changes in our day-to-day operations. The projects are slowly being rolled out, funded instead by SRMS/EDI.
What bothered us was that over the years some of the organizations receiving the bulk of the funding were faith-based and discriminated against some patients. While the projects themselves were potentially more neutral, the organizations were not. Health and Human Services (HHS) apparently looked only at the proposals in determining the awards, making the awarding of grants potentially flawed.
The grant process essentially compartmentalized the proposals. If an organization provided certain services, which the federal government did not fund directly, but the organization was awarded a grant to provide other services, the government essentially compartmentalized the grant money separate from the procedures it didn’t directly support. I understand the concept but do not feel the grant committees should have made the decision based only on the grant proposals. They also needed to take into account the overall views and beliefs of the organization requesting funding. There needs to be times when the government must look at the trees and not just the leaves.
I believe there were instances where the funds should be withheld. The funded organizations should have provided a minimum standard of practice guidelines in line with the non-discrimination clauses outlined in the grants. Entities awarded the grants should not have discriminated with regards to race, religion, ancestry, gender, marital status or sexual preference.
 Being a faith-based embryo donation/embryo adoption organization also directly or indirectly excludes some patients, making it uncertain if the federal government should directly support such facilities, especially taking into account the separation of church and state. I know that faith-based embryo donation/embryo adoption entities were strongly supported by past administrations but should a neutral organization that does not discriminate and makes all faiths feel totally welcome be placed at a higher priority now? Is this more ethical and fair? Is this a better use of the shrinking tax dollars? Is it time for the federal government to reconsider their goals?
Being a faith-based embryo donation/embryo adoption organization also directly or indirectly excludes some patients, making it uncertain if the federal government should directly support such facilities, especially taking into account the separation of church and state. I know that faith-based embryo donation/embryo adoption entities were strongly supported by past administrations but should a neutral organization that does not discriminate and makes all faiths feel totally welcome be placed at a higher priority now? Is this more ethical and fair? Is this a better use of the shrinking tax dollars? Is it time for the federal government to reconsider their goals?
If both discrimination and faith-based issues were actually taken into account, many of the organizations discussed here never would have received the original federal funds.
It is not that I want these organizations to go away. Quite the contrary, they often do a great job, provide excellent services and fill a much-needed niche. Their funding should, however, be through sources other than the federal government because of the bias inherent to their provision of services.
Can the Government Afford Providing the Grants?
Understanding that the U.S. is running a severe deficit, when are we ever going to be  willing to make difficult decisions? How are we ever going to get control of the budget if we can’t trim existing programs that may serve an important few when the many need assistance? We all need to look at the big picture and understand that “business as usual” is not practical in the current economic climate. I may be falling on the sword a bit, but shouldn’t we all be willing to sacrifice? Hey, I’m all for creating little taxpayers to help pay off the deficit. I’m just not sure that we can afford to do so through a government in the red. To do so with organizations that discriminate makes absolutely no sense at all.
willing to make difficult decisions? How are we ever going to get control of the budget if we can’t trim existing programs that may serve an important few when the many need assistance? We all need to look at the big picture and understand that “business as usual” is not practical in the current economic climate. I may be falling on the sword a bit, but shouldn’t we all be willing to sacrifice? Hey, I’m all for creating little taxpayers to help pay off the deficit. I’m just not sure that we can afford to do so through a government in the red. To do so with organizations that discriminate makes absolutely no sense at all.
In Summary
If federal funding is to continue, it needs to be provided to organizations, and not necessarily my own, which do not discriminate and are not faith-based. In addition, giving “embryo adoption” programs federal funds so they can support personhood amendments should be reconsidered. Having the government eventually spend even more money and time contesting the amendments and statutes in court defies understanding. Perhaps the congressional appropriations committees, who will make the final decision regarding federal funding, will take the concepts of non-discrimination and non faith-based alternatives into account and fund the programs with new and fairer goals.
Rest assured, unlike the rhetoric would lead one to believe, embryo donation is here to stay, regardless of the decisions of Congress and the grant process. How do we know? We’ve been providing the service for 11 years and will continue to do so in the years ahead, without cessation, as long as there are cryopreserved embryos available to donate.
Craig R. Sweet, M.D.
Reproductive Endocrinologist
Embryo Donation International
www.EmbryoDonation.com
2 Responses to “Federal Funding of Embryo Donation and “Embryo Adoption:” Is it time for the Federal Government to Reconsider Its goals?”
-
Dr. Sweet,
I appreciate what you have communicated here. Especially your summary.I’ve always had the attitude that self-reflection is a very important quality, especially in running a business or organization. In the past our government granted funding to primarily the same groups; some for five years. Perhaps the decision to pull funding was economic as well as a reality check.
Is the money spent accomplishing its goal? I would agree with you that when it comes to embryos, the greater population recognize the term Embryo Adoption because the funding has primarily been awarded to faith based groups with a greater outreach and an appealing message (apparently accuracy is not required).
I am thankful you, Embryo Adoption International are here to stay. You are a priceless benefit to Infertility patients.
How Does EDI Decide to Exclude Potential Embryo Recipients?

By: Craig R. Sweet, M.D.
Reproductive Endocrinologist
Info@EmbryoDonation.com
Introduction
There are times when we need to exclude patients when they contact Embryo Donation International (EDI) to become an embryo recipient. While not an easy decision or discussion, I thought it was time to explain our rationale when needing to, at least temporarily, exclude potential embryo recipients.
In a way, the blog we recently wrote on the ranking of potential embryo recipients dovetails into this discussion. In this blog, we described what we thought was an appropriate ranking system prioritizing those patients with the greatest need.
Our discussion here focuses on the patients who apply but who are never ranked because EDI feels they should be excluded because of any number of the reasons described below.
Excluding Potential Embryo Recipients Due to Maternal Risks
The decision to exclude a patient from embryo donation is really, in some ways, no different than the decision we have to make with other infertility patients.
Relative contraindications to pregnancy
There are occasions when certain conditions should probably be corrected before pregnancy takes place since pregnancy will often worsen or complicate the condition. Examples may include gallbladder disease and ovarian cysts or surface uterine fibroids that are five+ centimeters in average diameter. Treating these problems once pregnancy is established is very difficult, so it may be best to control the situation while we still can and correct the potential problem first before conception.
Strong contraindications to pregnancy
Patients who would be at significant risk of illness or even death should pregnancy occur include those suffering from cancer, poorly controlled systemic lupus, pulmonary hypertension or diabetes, to name a few important disease states.
Infrequently we have to be a bit paternalistic and say “no,” understanding that we may cause great harm to our ill patients by assisting them to become pregnant.
Excluding Potential Embryo Recipients Due to Risks to the Embryo/Fetus
The trickier decisions involve those patients where the potential for delivery of a live child is measurably reduced. Patients with decreased embryo implantation rates and those who are at an increased risk for spontaneous loss or at an increased risk for premature delivery/stillbirths fall into these categories.
Some of these examples are listed below:
|
Situation |
Decreased implantation |
Increased risk of spontaneous loss |
Increased risk of significant prematurity or stillbirth |
| Uterine cavity distorting fibroids or polyps |
x |
x | |
| Uterine fibroids 2+ cm in size located within the uterine muscle |
x |
x |
|
| Damaged uterine cavity with a thin endometrial lining |
x |
x |
|
| Hydrosalpinx where tubal fluid may flow back into the uterus |
x |
x |
|
| Unexplained recurrent pregnancy loss |
x |
||
| Uncontrolled medical conditions (e.g., hypertension, diabetes, renal disease, autoimmune disease) |
x |
x |
|
| History of an incompetent cervix |
x |
x |
|
| Persistent history of premature births |
x |
||
| Untreated pre-diabetes |
x |
x |
x |
| Obesity or morbid obesity* |
x* |
x* |
x |
* The effects of obesity or morbid obesity with regards to implantation rates and spontaneous loss rates are controversial.
The “Grey” Exclusion Zones
Out of the list above, one of the most difficult categories involves those patients who are obese or morbidly obese and their  potential reduction in implantation rates and increased spontaneous loss rates. Some articles show a significant reduction in implantation rates and an increased risk of spontaneous loss while others show contradictory results. While a comprehensive review of this topic goes beyond the scope of this blog, I believe there are a few things we understand:
potential reduction in implantation rates and increased spontaneous loss rates. Some articles show a significant reduction in implantation rates and an increased risk of spontaneous loss while others show contradictory results. While a comprehensive review of this topic goes beyond the scope of this blog, I believe there are a few things we understand:
- Patients with glucose intolerance and insulin resistance, regardless of weight, are at a higher risk of developing gestational diabetes during pregnancy and the potential complications associated with this disease.
- Patients who are obese or morbidly obese are clearly at risk during pregnancy for a host of issues, including preeclampsia, hypertension, large for gestational age babies, prematurity, stillbirths, gestational diabetes, Cesarean section deliveries and the risks associated with these surgeries.
There is only one preliminary study specific to embryo donation that did not show a consistent decrease in pregnancy rates as weight increased (Body Mass Index: BMI) but the trends were present suggesting an average reduction in overall pregnancy rate of 33% for obese and morbidly obese patients with a BMI of 30 or more. (Finger R., et al. 2011) We await the detailed publication of this important study to better understand this issue.
Weight loss is terribly difficult for patients and takes a great deal of time. Sometimes surgery, such as a gastric band or intestinal bypass surgery, may be the best option. These issues are the thorniest to decide, with pressure applied by potential embryo recipients who do not fully understand how their weight may contribute to failed implantation or pregnancy loss, though it certainly places them and their unborn offspring at greater risks during the pregnancy.
Surrogacy as an Option When Material/Embryonic/Fetal Risks are Too High
 Some of the issues discussed in this blog can be treated. Then the potential embryo recipient can be moved out of the exclusion zone. Some of these issues are not treatable, so options such as surrogacy and/or adoption may be better alternatives.
Some of the issues discussed in this blog can be treated. Then the potential embryo recipient can be moved out of the exclusion zone. Some of these issues are not treatable, so options such as surrogacy and/or adoption may be better alternatives.
While some embryo donation programs refuse to allow surrogacy, EDI feels this is an excellent alternative. For example, is it ethical for EDI to ask that the patient with asymptomatic uterine fibroids, which may significantly reduce implantation or increase pregnancy loss rates, be surgically removed in a patient who fears surgery? Is gestational surrogacy a better alternative?
In Summary
We do not mean to be cruel or judgmental but are forced to make difficult decisions regarding the acceptance or exclusion of embryo recipients. We owe it to the potential embryo recipients to give them the best chance possible, understanding there are medical conditions that may severely impair their chances for success. We owe a debt of gratitude to the embryo donors and take seriously the responsibility of finding a healthy patient for their embryos hoping to maximize the chances that the embryos will survive and thrive. Lastly, and certainly not least, we owe it to the embryos to make certain they have the best chance possible.
Unfortunately, we sometimes have to make the difficult decision to exclude a potential embryo recipient, at least temporarily, until the medial concerns are remedied or certainly improved.
References:
Finger R, et. al. Obesity and the ability to achieve pregnancy in embryo donation. Fertil Steril 2011;96(3)-S172.
4 Responses to “How Does EDI Decide to Exclude Potential Embryo Recipients?”
-
With respect to the potential recipent who has had a past history of fibroids reoved from the uterine cavity, are they excluded permentantly due to the history of fibroids, or just while the fibroids are in the uterine cavity? Once they heal from their chosen treatment method are they allowed for consideration if they are deemed to pass your health criteria?
-
We are exploring the option of embryo donation due to years of unsuccesful IVF/ICSI treatment. We live in NZ, would we be excluded from your programme?
-
I am looking for donor embryos. I am of an age that REs will not work with me. My husband and I are willing to get a surrogate to carry the pregnancy. I have had several IVF cycles and have been told that my womb will not hold a pregnancy. My husband and I have tried for many many years to have a family, we are from the UK so have few options avalible to us. We would need a US surrogate with a US clinic using donor embryos. Is this something that would be avalible to us.
Parent via Egg Donation – Parent via Embryo Donation

Marna Gatlin of PVED
Exploring what we know – Marna Gatlin, Founder Parents via Egg Donation and guest blogger
I was asked recently what I thought about embryo donation vs. egg donation. Is a parent via egg donation the same as a parent via embryo donation? What do they have in common? Or are they very different?
My knee jerk reaction was “Well doh, of course they are the same. They are both embarking upon a unique journey to become parents right?”
When I thought more about it, the word “versus” jumped out at me. Did the individual asking the question really mean “versus” as in against, or in contrast to?
Are the two mutually exclusive?
When I think of egg donation and embryo donation, I think about the word “AND” – I don’t think of it as an either or. Both are just different ways of either growing or adding to your family.
Some approach embryo donation with great trepidation because they worry about the bonding process, or about the explanation or story they will be sharing with their child. The reality is – the path might be different but at the end of the day the goal is the same – you are becoming a parent.
Let’s delve a little deeper. If you receive a donor egg, the genes of your baby are going to be combined with the genes of your husband (or partner) and those of your egg donor. Or if you are a single mother, or women in a same sex relationship, the donor egg will be combined with donor sperm. You will probably undergo what we call a fresh embryo transfer. You will carry that baby for nine months and then deliver that baby. Women often wonder if there’s a down side to carrying a baby that is not genetically related to them. You know this is an age old question that’s been asked and answered since the early 80’s when the first donor egg child was conceived, carried, and delivered. I can tell you as a parent via egg donation myself that it doesn’t matter. I carried my son for nine months. The bond I created with him is rock solid, loving, and he’s my son. The lack of genetic connection simply doesn’t matter. Not one iota. The very same thing happens with embryo donation recipient parents who are receiving truly a meaningful gift of life.
genes of your husband (or partner) and those of your egg donor. Or if you are a single mother, or women in a same sex relationship, the donor egg will be combined with donor sperm. You will probably undergo what we call a fresh embryo transfer. You will carry that baby for nine months and then deliver that baby. Women often wonder if there’s a down side to carrying a baby that is not genetically related to them. You know this is an age old question that’s been asked and answered since the early 80’s when the first donor egg child was conceived, carried, and delivered. I can tell you as a parent via egg donation myself that it doesn’t matter. I carried my son for nine months. The bond I created with him is rock solid, loving, and he’s my son. The lack of genetic connection simply doesn’t matter. Not one iota. The very same thing happens with embryo donation recipient parents who are receiving truly a meaningful gift of life.
The most beautiful aspect of embryo donation to me is that embryos that are being placed for donation are done so purposely. These are embryos that the donating parents know have created amazing children who are loved, honored and cared for. These donating parents want to make sure their embryos are donated to a home that will love, cherish and honor the resulting children as they would. Regardless of whether an individual has a child via egg donation or embryo donation, the fears of parenthood almost always focus on the unknowns. And here’s a secret: they are also experienced by those who are conceived naturally. Moms and Dads all over the world have the same worries about parenting as do parents via egg donation and embryo donation.
Parents via egg donation often ask questions such as:
- Am I going to screw up my child?
- Will my child love me?
- How am I going to relate to my child?
- Will my parents and other family members accept my child?
- How and when will I share information about their conception?
When we look at embryo donation the questions that we find unique to embryo donation are:
- Are we protected legally, can the donating parents come back and claim our child in the future? (The answer is NO, they cannot. That’s why it’s important to have a clear legal contract.)
- Will my child have access to information about his or her health in the future?
- Will my child have siblings and if so, will they have the opportunity to know them?
- Will my child or children see me as their real parent?
- How will I explain this to my family or friends?
- What about stupid comments from those around me?
- How and when will I share the information about my child’s conception with my child?
To me there is no difference between being a parent via egg donation or a parent via embryo donation. The end result is the same.
At the finish line we are simply Mom and Dad.
Marna Gatlin
Parents via Egg Donation
www.PVED.org | marna(at)pved.org
A little bit about Marna…
After many years of struggling with infertility, PVED founder Marna Gatlin discovered that the technology to have a child through egg donation was available. She was curious, excited, and above all, hopeful that this process might be the conduit to finally achieving her lifelong dream of becoming a parent.
Marna ensures that all the needs of egg donor recipients are met, maintaining a high standard of ethics and confidentiality. Marna advocates and assists recipient parents, helping them arrange for the highest quality patient care, wherever in the world they reside. Her experience and knowledge related to the complex emotional and physical needs of individuals dealing with infertility makes her an essential asset PVED.
As a previous recipient, Marna is uniquely qualified to provide caring and timely services. Marna is truly dedicated to compassionately guiding couples experiencing infertility through their treatment process.
Marna is joined by several dedicated and knowledgeable support staff that all work together clearly dedicated to see the success of PVED. These include clinical psychologists, reproductive endocrinologists, attorneys, as well as a talented business and public relations team.
Marna attended Eastern Oregon University and Portland State University majoring in Business, Psychology, Social Science, and is a member of the American Society of Reproductive Medicine (ASRM), the European Society of Human Reproduction and Embryology (ESHRE) and the Society for Assisted Reproductive Technology (SART). Marna, a writer, is married, has a son, and does some of her best thinking and creating atop of her John Deere tractor mowing and cultivating her back forty.
One Response to “Parent via Egg Donation – Parent via Embryo Donation”
-
Excellent commentary, Marna. I agree 100% with your views. In the end, it’s all about realizing your dreams of becoming parents!
Final Post in Mini-Series: Thawing/Warming Embryos
 In the first two segments of this series, we discussed embryo grading and cryopreservation (1 – Do these embryos make the grade? and 2 – Embryo Cryopreservation: An Easy to Understand Review). This final segment in the series will examine the process of thawing or warming of embryos for transfer.
In the first two segments of this series, we discussed embryo grading and cryopreservation (1 – Do these embryos make the grade? and 2 – Embryo Cryopreservation: An Easy to Understand Review). This final segment in the series will examine the process of thawing or warming of embryos for transfer.
In Review…
Let’s begin with a short review of the previous blogs. You will recall that we discussed two methods of embryo cryopreservation, slow freezing and vitrification. Both methods require that the cells of the embryo have as much water removed as possible and that cryoprotectants, materials that protect the cells during freezing, be forced into those cells to reduce ice crystal formation. Slow freezing uses a controlled rate freezing instrument that slowly lowers the temperature to well below freezing to avoid the formation of ice crystals. Vitrification is a method in which embryos are plunged directly into liquid nitrogen and immediately turned into a glass-like substance, essentially cooling the embryos so quickly that ice crystals do not even have time to form.
Cryopreservation Storage Containers
One topic not covered in the freezing blog was the type of containers used to hold the embryos. Slow freezing, in most cases, uses straws or vials to hold the embryos in a small amount of solution called media. Vitrification uses many different storage devices to hold the tiny embryos, which cannot be seen without a microscope. These devices commonly include various types of straws, nylon loops or electron microscope grids, just to name a few.
How Often do the Cryopreserved Embryos Survive?
It is expected that about two-thirds of embryos cryopreserved via a slow freeze technique will survive thawing (Son and Tan, 2009) and the embryos that do not survive are most likely genetically abnormal. For embryos that are vitrified, the rapid cooling/warming process seems to work better, with about 80-90% of the embryos surviving. For this reason, vitrification is becoming more popular for cryopreserving both eggs and embryos.
How Many Embryos Should Be in Each Container?
Ideally only one or two embryos should be packed into each storage container. By packaging one embryo per container, the embryologist can thaw or warm only the exact number of embryos to be transferred without having any left over. For example, if a patient wants to have two thawed cryopreserved embryos transferred and they have a total of five embryos each frozen in separate containers, the embryologist will thaw/warm one container at a time until just two healthy embryos are recovered. If, however, the same five embryos were packaged in two containers with three embryos in one and two in another, the embryologist would probably first begin thawing/warming the container with three embryos. Should all of the embryos survive, there is one excess embryo that would need to be transferred, refrozen or discarded. While recent studies have indicated that freezing embryos a second time can result in a pregnancy, particularly when using vitrification, it is ideal to only thaw the exact number of embryos that we want to transfer and not one embryo more. (Kamasko, Y. et.al., 2009).
How are the Embryos Thawed/Warmed?
Ice crystal formation is also the enemy when thawing embryos, just as when cryopreserving them,. As embryos warm from -196°C (-321°F) toward 0°C (32°F), ice crystals may again form and damage the cells. We use the following techniques to rapidly warm/thaw both slow frozen and vitrified embryos in an attempt to avoid ice crystal formation:
- For embryos frozen by the slow freeze method, the straws or vials are removed from the storage tank and held at room temperature for 30-60 seconds, allowing the embryos to warm only slightly. The storage container is then plunged into 37°C water, completing the thawing process quickly enough so that the ice crystals don’t have a chance to form.
- Vitrified embryos are taken out of liquid nitrogen, with the container then plunged directly into warming media that is either at room temperature or 37°C, depending on the method used to vitrify the embryos. Once again, the ice crystals simply do not have enough time to form.
Once the embryos have been thawed/warmed, the cryoprotectants that replaced the water in the cells must be removed and balanced solutions placed back into the cells. To accomplish this, embryos are moved from small bath to small bath with varying concentrations of water and other substances. As the cryoprotectants are removed, the cells fill with water containing the nutrients and growth factors needed for cellular recovery. Once the embryos have been thawed/warmed, they are placed in the incubator in supporting culture media for two to twelve hours to allow the cells to continue equilibration prior to transfer. If we are thawing embryos that were frozen early, we may even grow the embryos for a few days so that we transfer the fewest healthy embryos we need to achieve a successful pregnancy.
Are There Other Factors That Influence the Survival of Cryopreserved Embryos?
While ice crystals play a big role in the survival of embryos, they are far from the only concern. Embryo survival rates vary for many reasons including;
- Embryo quality: Poor quality embryos freeze and thaw poorly. Poor early development of an embryo suggests that the embryo is in the process of dying and such embryos should probably not be cryopreserved.
- Freezing media and cryoprotectant “recipes“: Some recipes are potentially better than others and each laboratory has to find which works best. What works well for one, may not be the best for others.
- Laboratory techniques: Laboratories must have an excellent quality control program to assure they are following the steps involved in freezing/cooling and thawing/warming the cryopreserved embryos precisely.
- Embryologist variability: As with all techniques that involve humans, some seem to do a better job than others. There is no substitution for careful training and experience.
In Closing…
We hope this series has given you a glimpse of what is involved in grading, freezing/cooling and thawing/warming your precious embryos. Cryopreserved embryos give patients the option to build their families in a cost effective manner. Without cryopreservation, embryo donation would really not be possible.
Corey Burke, B.S, C.L.S.
Laboratory Supervisor
Embryo Donation International
CBurke@EmbryoDonation.com
References:
Kamasko, Y. et.al. The efficacy of the transfer of twice frozen-thawed embryos with the vitrification method. Fertil Steril 2009;91:383-386.
Son, W.Y., and Tan, S.L. Comparison between slow freezing and vitrification for human embryos. Expert Rev. Med. Devices 2009:6(1),1-7
Embryo Cryopreservation: An easy to understand review
Why are Embryos Cryopreserved?
Infertility patients invest so much time, effort, money and emotion into each IVF cycle. After the fresh embryos are transferred, about 30-40% of our patients will have excess high quality embryos available for freezing, also known as cryopreservation, to be used for future cycles. Frozen embryo transfers are a cost-effective way to pursue further treatment, regardless of the outcome of the fresh embryo transfer cycle.
Patients are often curious about the methods their laboratory uses to freeze their embryos. Cryopreservation is a delicate process requiring extensive expertise to prevent damage to the embryos during the freezing and thawing procedures.
Preventing Potential Damage During Freezing
There are three major types of injury that can occur to cells during the cryopreservation procedure (Jain JK, et al., 2006):
- (i) Exposure of cells to ice crystal formation during freezing and/or thawing;
- (ii) Damage to the embryos from the solutions used to prepare the embryos prior to freezing; and
- (iii) Damage to the embryos as water and electrolytes shift in and out of the cells that make up the embryos.
Damage from ice crystal formation is overcome by removing as much water from within the cells making up the early embryo and replacing it with fluid containing cryoprotectants. To remove the water, embryos are placed in a series of solutions using increasing concentrations of salt to draw the water out of the cells. Once this is accomplished, the embryos are then placed into additional solutions containing the cryoprotectants, which enter the cells taking the place of the water.
Removing the water from the cells is relatively simple while replacing the fluids with cryoprotectants is a bit more difficult and damage to the embryos can occur if not done correctly. Cryoprotectants can be toxic to the embryos, so the cells can only be exposed to them for a very short time before they are frozen. Once the cells have been filled with cryoprotectants, cryopreservation needs to take place fairly rapidly.
Slow Freezing and Vitrification Techniques
The two most common cryopreservation methods used to freeze embryos are slow freezing and vitrification. The slow
freezing method has been around for decades. Slow freezing involves loading the embryos into special straws or vials and placing them in a separate container, which is surrounded by a liquid nitrogen bath. The container controls the rate of temperature drop and freezes the embryos slowly over a few hours, preventing most ice crystal formation. The freezing device lowers the temperature gradually to -38° C. Once the embryos have reached this temperature, the vial or straw is plunged into a bath of liquid nitrogen to reach a final temperature -196°C (-321°F). They will remain at this temperature until they are thawed.
With vitrification, embryos are rapidly cooled to -196°C (-321°F) almost instantly. This instant cooling does not allow ice crystals to form. Vitrification comes from the Latin vitreum, meaning the transformation of a substance to glass. Please note the use of the word “cooling” is used rather than “freezing” when referring to vitrification. Freezing actually involves transitioning a liquid to a solid through crystallization. No crystals are actually formed during vitrification. To understand the difference better, take a look at an ice cube from your freezer. While it is mostly clear, you will notice it is somewhat cloudy due to ice crystal formation and not as clear as glass. Water that is vitrified appears absolutely clear because ice crystals never had the chance to form and a glass-like substance is created.
Vitrification still requires the replacement of water with cryoprotectants but uses a different recipe. In fact, the cryoprotectants used for vitrification are at a higher concentration and potentially even more toxic to the embryos. Once the embryos are exposed to the high concentration cryoprotectants, they must be frozen very rapidly. Whereas the slow freeze process takes place over hours, vitrification takes place over minutes.
Is One Cryopreservation Technique Better than the Next?
The process of embryo vitrification is relatively new compared to the slow freeze method; however, great advances have been made over the past decade.
There is evidence that vitrification is a slightly better system than slow freezing. In most studies, the embryo survival rates are better for vitrification than the slow freeze technique. A recent study by Kaskar, K. et.al, also showed that the pregnancy rates with vitrified/warmed embryos (64%) were significantly higher than those that were frozen/thawed by the slow freeze techniques (47%). With higher survival rates and higher implantation rates, vitrification is slowly replacing the slow freeze technique, especially for the storage of eggs and embryos.
Success with Re-vitrification
Vitrification may allow embryos to be warmed, re-vitrified, and warmed again with successful pregnancies reported. While the pregnancy rates are somewhat lower that that of embryos vitrified only once, the results are far better than embryos slow frozen, thawed, re-frozen, and thawed yet again. A 2007 study by Kamasko, Y. et.al, showed no significant differences in implantation rates between once vitrified embryos and twice vitrified embryos. The reason this is important is that embryos may be frozen/cooled in groups larger than we want to transfer. For example, if a patient succeeded with a twin pregnancy with two fresh embryos transferred and only wants one frozen embryo transferred for a future child, having two cryopreserved embryos survive that were stored in a single vial would present a problem. In this case, we would possibly transfer more embryos than we wanted to, discard the extra embryo (not at all desired) or refreeze/re-vitrify the extra embryo. Using vitrification, the embryo may indeed survive a second stage of warming for an additional pregnancy in the future.
Your Embryos Are Very Important
As embryologists, we take our responsibilities to care for your cryopreserved embryos very seriously so that you will have the opportunity to use them for future treatment cycles. Rest assured they will be available when you need them, having been cryopreserved with the most state-of-the-art techniques at our disposal.
Thawing/Warming Your Embryos
If you would like to learn about how embryos are thawed/warmed, be sure to watch for our upcoming blog on this topic!
References:
Kaskar, K., et.al. Comparison of clinical outcome of blasocyst vitrification with slow freezing and fresh embryo transfer. Fertil Steril 2010;94:113-114Jain JK, Paulson RJ. Oocyte cryopreservation. Fertil Steril 2006;86(Suppl 3):1037-46.
Kamasko, Y. et.al. The efficacy of the transfer of twice frozen-thawed embryos with the vitrification method. Fertil Steril 2009;91:383-386
One Response to “Embryo Cryopreservation: An easy to understand review”
-
sdfdssfs





Dear Dr. Sweet,
Thank you for all the time, thought and dedication you put into discussing this important issue in an open forum. This is an incredibly important issue, and I hope many people are taking the time to consider it.
Being a person who believes strongly in reproductive freedoms, it is difficult for me to be critical of anyone’s choices when it comes to reproductive technologies. However, that is the exact crux of the matter – it is the reproductive freedoms of the users of assisted reproductive technologies that we must safeguard, and not the freedoms of the medical community to make embryos as they see fit.
Thank you Sara.
I do truly feel that California Conceptions really didn’t want to just make embryos. They just wanted to help their patients. At issue are the unintended consequences of their decision. No matter what they do, they will create an embryo bank that will be owned by CC. Unless someone can provide an argument against, I simply feel embryos should only be owned by patients and not a business, corporation or physician practice. Who else should be deciding their fate than those that took on the responsibility of their creation?
Thank you Dr. Sweet for this well researched and supported argument against the banking of embryos. It seems to me that the infertility profession must be extraordinarily careful with any appearance of treating the creation of embryos callously. And even if that is not the intent of embryo banking, no matter how small the bank, the hint of impropriety could do great damage to the profession, and most important to the legends of infertility patients.
Dawn Johnson
Creating a Family ~Education and support for infertility and adoption
Dawn:
I totally agree with your concerns. The potential for harm to women’s health care and the infertility world could be great if embryo banks are taken up as a rallying cry to those that would prescribe personhood to embryos.
Thank you, Dr. Sweet, for writing such a well-researched compilation of this issue, from your perspective as well as many others. I have written my own thoughts on this for the Choice Mom community of single women who use embryo donation, among other methods, to build families. Here’s some of what I said: “We like to trust those businesses who help us build our families using the amazing new methods of reproductive technology. But, we’ve heard stories of how those technologies have been misused, even by well-meaning doctors. I’m not in favor of letting a commercial business decide which lovely egg donors and which prolific sperm donors they will combine, unsupervised, to create the best package of fully related children The Market Wants. I am highly in favor of embryo donation for the Choice Mom community, but with parameters that keep our eventual offspring in mind. As always, how will they feel about their origin story?
Mikki:
Thank you for your very thoughtful comments and your wonderful blog.
While I don’t feel that California Conceptions (CC) was making any embryos without clear consent from recipients regarding the choice of the egg and sperm donors, we absolutely run the risk of others creating “McEmbryos” placing egg and sperm donors together based on market research, personal preference all significantly focused on the greatest likelihood for profitability. If all the cryopreserved donor/donor-conceived embryos find a home, I have less to complain about. What happens, however, if some of the cryopreserved embryos are never chosen? Who will decide their fate? Who should decide their fate?
Dr. Sweet – I first want to thank you for your time, dedication and bravery for writing a well-researched blog from your perspective as well as sharing the ideas and thoughts of the many others you have referred to in this piece.
The practice of creating “ready-made embryos” has been going on for a very long time, at least to my knowledge since 1997. Last year (2012) the subject came up again and tongues were wagging over the fact that California Conceptions was reportedly creating embryos from donor eggs and donor sperm and then taking those embryos and distributing them to their embryo recipients and saying this was “embryo donation” when really it’s not. In fact, what I think California Conceptions is really doing is creating embryos from donated eggs and donated sperm with NO SPECIFIC RECIPIENT PARENT IN PLACE which means this clinic is creating embryos (picking and choosing genetics), banking them, and then selling them to patients with a money back guarantee.
Also, from my understanding is that any left-over embryos that remain from any cycle at CC are cryopreserved, placed back in the freezer and are owned by California Conceptions. Not the egg donor, not the sperm donor, and certainly not the recipient parents.
What does this mean?
This means that the original parents of these embryos are the CLINIC not the recipient parent.
I was one of the many who were contacted by a reporter from the LA Times to ask my opinion about the practices of “ready-made” embryos. I gladly spoke to this journalist as I felt I had something worthwhile to say as the Founder of Parents Via Egg Donation and as a mother via egg donation myself. Unfortunately none of what I had to say made it in the LA Times piece and it’s a shame really because I think as a parent and a leader of a rather large egg donation community our thoughts and opinions had validity.
First of all let me say that you can’t put a price on a life, however, we all as patients pay a lot of money for to clinics and agencies to help us with creating our families. I can understand why the program at CC would be incredibly inviting because of the price structure but my biggest problem with all of this is that from what I am to understand this clinic is selecting egg donors and sperm donors and putting them together and then SELLING those embryos. However, this really sounds like to me like “pre-destination embryos” and in my book that’s a problem. I also understand that CC was trying to offer a better solution – or a more economical solution as an alternative to patients. However, I don’t care if the intent of the embryo bank was to be small or large it’s still a commercial embryo bank and that’s not okay. These folks are not storing left over embryos from previous patients who are trying to decide if they want to add to their families, these are embryos to be sold.
I think we need to be clear – this is NOT embryo donation. It’s not. It’s not. It’s not. These are embryos that are created, hand-picked, & specifically created by California Conceptions. It’s akin to a mail order bride, but it’s a potential mail order kid.
Doesn’t that leave a bad taste in your mouth?
The saddest piece to all of this is that there are hundreds of thousands unwanted cryopreserved embryos that are on ice all across the USA. Over 500k to be exact. My guess is that many of these embryos could be donated to couples all over the globe if the donating parents knew that donation was clearly an option. Education is key.
Aside from the whole disgusting commercialization piece to all of this what about the kids? Hasn’t anyone thought about the kids? If a cycle split between 3 couples creates three, four, five children, all these children are going to be genetic siblings who are NEVER going to know about one another. And that in my book is irresponsible and unconscionable.
In closing I am all for thinking outside the box. I am open minded about how family can be or should be created. However, this program I don’t think has thought this through and if they have shame on them. Nothing about this program can be justified, morally or ethically.
As the leader of PVED I work very hard to bring egg donation to the forefront and present it as not being “weird” or something from outer space. I justify what we do to those who would like to ban egg donation, embryo donation, and anything third party every single day. I answer questions daily in regards to egg donation and is it really creating designer babies, and is egg donation or embryo donation ethical. However, its stuff like this that will indeed give those who support personhood a leg to stand on and will indeed bring regulation faster than you can create an embryo.
Physicians should not be allowed to intentionally create and market embryos. There are so many things we already customize – houses, landscaping, boats, cars, — children should not be one of them.
Marna:
You make some wonderful points. Your perspective is valued and highly respected.
Continuing your thinking outside the box, there are compromises that could entertained by California Conceptions would allow them to care for their patients with few changes. All they have to do is to make certain that all excess cryopreserved embryos are owned by one or more of the recipients. I think it is really that simple.
The points made regarding the genetic siblings not likely to connect is a concern that is ringing true throughout the donation word, thus the push towards open identity options. Let’s be honest, though, CC isn’t the only one that could be criticized on this issue.
I suspect what leaves you with such a bad taste is the minimal level of respect the embryos seem to garner. It is as though we were dividing home-made cookies amongst a group of three, four or five with the extra cookies kept by the original baker to hopefully be given to others at some later date. I would not want my embryos to be treated as such and I can’t help but wonder if the caring physicians at CC might feel the same as I if it was their genetics that were used to bake the cookies in the first place….
Thank you Dr. Sweet for bringing this conversation to a public forum. I share the concerns shared by others in this forum. As I continue to think about this topic, I only have a few comments to share.
1. The CC option is, in part, a market response to a rare resource. Embryos that are available for adoption to patients represent only 2.3% of all the stored embryos in the US– see this Rand Study http://www.rand.org/pubs/research_briefs/RB9038/index1.html The vast majority of embryos (over 88%) are stored for the patients who created them for their own use and will likely never be donated. As a lab director, I found this to be true on a smaller scale at every lab I directed so I believe these percentages. Greater education may help in some clinics but we took great pains to make sure all options were explained and available to our patients and still only a relatively small number chose to donate their embryos to other patients. We need to work harder to ensure affordable access to high quality infertility treatments for all patients–this would make these “bulk buying” arrangements to acquire embryos unnecessary and unappealing.
2. I agree that ART labs/clinics/professionals really need to stay away from practices that result in “owning” embryos. It’s hard (impossible?) to thread that needle without being subjected to accusations of commodification of embryos.
3. Finally, I always circle back to one nagging issue. All of my career in ART, our focus has always been solely on satisfying the immediate needs of our patients to achieve a pregnancy.In most cases, we were simply bypassing natural barriers by providing IVF services so couples could conceive their own children-with a little help in the lab. Then we worked with donor gametes that couples chose to conceive their own “intended” children. We profit from all these interventions. Now clinics are going further to address our client’s needs –supplying unrelated embryos to couples–either from embryos donated by other patients or embryos created with the intention of being donated or adopted- and in some cases having left over embryos. I think these latter “embryo matching/ embryo donation” advances place a greater burden on the IVF programs to give some thought to providing these services within a framework of transparency– so that donor-conceived children have an option in the future to have some information about their biological origins. IMO, we need to think about embryo donation registries as well as sperm and egg donor registries. Donor conceived children are speaking up –loudly and angrily in some cases- about the fact that at the time of their conception, no one gave any thought to their future emotional or medical needs for having some connection to their biological roots. Due to poor records and preferential recruitment of donors who favored no strings donation, kids often have no realistic chance of finding their bio-relatives. I don’t think we have a right to decide for every donor-conceived child in advance that they don’t need this access. I think that is one step too far. I would like to see this discussion about embryo donation also include some consideration about the place of registries as we move forward full-speed with providing more unrelated embryos to more couples- in one fashion or another.
Dr. Sweet:
I appreciate the challenge to articulate why the practice of embryo creation and banking as described is objectionable to me as a mental health professional, family advocate, and mother of an adult son conceived long ago through ovum donation.
The litmus test on ethics in reproduction should begin with the question “what do we tell the kids? What is this story? How do we build families non-traditionally that make psychological sense?”
The story we can tell our children thus far with our various methodologies of reproduction is that people who plan to be parents select gametes and a uterus. They select medical facilities. Gamete providers are chosen for various reasons, both emotional and simply logical, but are chosen by PARENTS who don’t have children yet. They make choices about who they are going to make a baby with, just as people do who conceive in the bedroom, but removed from one’s own genetics. We can tell our kids that “mom and/or dad decided this or that and we got you.” Those decisions are the first decisions parents make on behalf of the children they don’t yet have.
Individuals who are donor conceived with sperm from cryobanks are returning to those cryobanks by the hundreds to request information or contact with previously anonymous donors. Can we learn nothing from history? What of the children conceived not by their parents but by a corporation with little or no interest in the psychological outcome?
In truth, those of us who have been thought leaders in this field, are just now figuring out the story to be told to offspring of “conventional” embryo donation. It’s a tough story. The embryo was conceived by a family who (usually) had children and then gave the (leftover) embryos to someone else. There are lovely ways to frame this story, as it is indeed always altruistic, and with the intent to give someone the opportunity to parent whose efforts have been otherwise thwarted. But there are issues of full siblings raised apart, issues of the randomness of laboratory procedures, and other issues that require extreme sophistication and conscientiousness on the part of both donating and receiving parties to address with any children in either family.
If you take the above issues and add to it the random selection of gametes chosen by personnel, not parents, and the issues of “ownership” and rights and everything that has been previously mentioned and we have a scenario that is extremely difficult to help children understand. The story has to make psychological sense and this story cannot because it does not.
It is my opinion that this practice is not contributing to the creation of healthy families.
Carole LieberWilkins, M.A.
Licensed Marriage and Family Therapist
Los Angeles, CA
Carole LieberWilkins:
I couldn’t agree with you more. While I do suspect any child conceived from an embryo bank would inevitably be loved and cherished, I too would wonder what my parents were thinking when they chose my genetic parent’s characteristics over all others. Above all, I would wonder about my genetic parents and my potential full siblings living other lives separate and detached from mine.
Carole,
I think registries would be welcomed by most clinics, though difficult if not impossible to administer. People move, change numbers, and don’t respond to phone calls. How is the registry funded so they can maintain contact with donors? Does the registry simply release a name or a social security number? What’s the clinic’s responsibility to track donors into the future and could they end up punished or sued if they don’t maintain contact? To compound this issue, most donors prefer not to be contacted. We ask about future contact using multiple questions and scenarios and I’d say that 90% or more say they do not want to be contacted. If regulations were to force this contact, it could certainly reduce the number of people willing to donate. Everyone seems to look at this from the perspective of the children, and I agree that needs to be considered, but the wishes of the donor should not be disregarded in the process. A tough topic and would make for a great blog post by itself.
Carole:
Regarding the 2.3% of all cryopreserved embryos donated to patients in need statistic, I think it is a bit low. Most publications on the topic quote a higher percent but certainly less than 10%. In my separate practice, Specialists In Reproductive Medicine & Surgery, a recent review revealed that 19% of our cryopreserved embryos were donated to patients in need. I think this is due to our hard work in educating the patients very early in the ART process as well and repeatedly in the future years when they really have to make the difficult disposition decisions. I should also state that we are a “non-destruct facility” meaning that we offer all options for the cryopreserved embryos other than discarding them. All IVF patients are well aware of this before they start the process and I have never received push-back” from patients who feel their own embryos are indeed precious and that they would never consider discarding them. Unfortunately, we know better. I believe continued cryopreservation, donation to the laboratory for QA work, donating to human embryonic stem cell research and donating the cryopreserved embryos to patients in need are plenty of options to provide the patients. It has always bothered me that one-half of the cryopreserve embryos would not be used by the patients who created them with a total of one-third being abandoned or discarded. I feel we need to gently guide patients toward better choices and what we do seems to work.
The concern regarding registries is important but very complex. It would appear that we are not going to form any type of registry anytime soon unless it is legislated at a state or national level. So many questions would need to be asked and answered before we could take this on. Your excellent moderation of this same concern on LinkedIn’s Embryo Donation Network garnered the largest number of comments to date (n=57) from people from around the world. We could learn so much from our peers in the Netherlands, Sweden, Finland, Austria and the United Kingdom. A wonderful review on this topic is available at the Social Science Research Network with a paper written by Sonia Allan titled “A Cross-Jurisdictional Study of Regulatory Requirements and Practice Regarding the Recording of Donor Information and Its Release to Donor Conceived People.”
Let me make it clear, however, any criticism levied against the California program regarding the lack of a registry should probably be levied against the vast majority of egg/sperm/embryo donation programs.
Dr. Sweet:
Thank you for the excellent post. I want to start off by saying that I fully support family building options using both donor sperm and donor eggs, and that I also support industry creativity in achieving lower cost options for patients. However, as with any treatment options, there are some moral, ethical and legal boundaries that should not be crossed. In that vein, I would like to discuss two of your points in more detail.
Terminology:
Embryo donation, in which excess embryos remaining after the conclusion of treatment are donated by former patients to others, has become a very attractive family building option for many intended parents. Some prefer embryo donation due to the relatively low cost; others see using existing embryos as a more morally acceptable option to using technology to create new embryos. However, California Conceptions’ model is not based on “embryo donation,” but rather “embryo creation.” Yet, the clinic persists in defining its model as “embryo donation.” The clinic’s website is filled with references to “embryo donation” and absent are references to the actual use of “egg donors” or “sperm donors” in their protocol. A few examples:
1. “But unfortunately, both traditional adoption and using an egg donor are very expensive and time consuming ways to build a family, especially after spending thousands of dollars on failed IVF cycles. Using Donated Embryos is Affordable and Combines the Best Aspects of Egg Donation with Adoption.”
These two sentences certainly give the impression that California Conceptions is not using egg donors in its program. This is not accurate–the model, as described by Dr. Zeringue is based entirely around egg donation.
2. “Anonymously donated embryos are a very affordable alternative to egg donation and adoption with similar benefits.”
This sentence clearly states that embryos are being donated. In reality, the donors are providing only eggs and sperm. While some may say this distinction is meaningless, in reality it has tremendous import. Those intended parents who are morally opposed to the creation of new embryos would have no way of knowing that the clinic is doing exactly that.
3. “Much like an anonymous adoption, embryos from IVF procedures are donated to couples and individuals wanting to have a baby.”
Again, the language is (deliberately?) phrased in such a way so as to mold the program to the traditional embryo donation model where a couple undergoes IVF and then donates their excess embryos.
4. “This donor embryo transfer is similar to using IVF with an egg donor for getting pregnant.’
No, California Conceptions model is not “similar” to using an egg donor; it IS using an egg donor. Why the need to hide that?
5. “Let us know how ready you are to proceed with embryo adoption.”
“Embryo Adoption” has been a term used exclusively to describe the donation of already-existing embryos. Even the most fervent crusaders determined to give every frozen embryo a chance at life don’t use the term “adoption” in relation to eggs or sperm.
6. “Do you have any strict requirements (other than healthy donors) when it comes to matching embryos to your profile?”
This language of matching “embryos” implies that embryos—and not eggs and sperm individually—are being matched.
Whether California Conceptions is deliberately misleading patients or whether the deception is just poor marketing choices on their part, the bottom line is that the potential for patients to be misled exists. I have heard the claim that California Conceptions fully explains the program to all patients—even if this is true, it does not balance out the potential for deception in their advertising materials. The double donor method used by California Conceptions is a perfectly legitimate family building option. Thus, I have to ask California Conceptions–why the need to disguise the method as something else?
And I have to wonder, if the marketing materials aimed at intended parents are deceptive, what about the marketing materials aimed at donors? Are donors providing full informed consent? Those of us in the industry know how dangerous it can be when donors are not fully informed of the process. Not only is lack of informed consent harmful to the donor, but it is harmful to the intended parents. Consider the situation in Options National Fertility Registry v. Dr. Michael Allon, Jud.Dis.190th, Harris Cty, TX (2005), where the egg donor did not realize that her eggs would be split between two couples. When the egg donor discovered this, she successfully sued to stop the donation to the second couple, even though the eggs had already been fertilized with the husband’s sperm. These are the kinds of situations that can arise when a clinic does not obtain proper informed consent from a donor.
Embryo Banking:
New York State has the right idea. Embryos should not be created except at the request of an identified patient(s). To do otherwise cannot be justified because the physician’s role is to assist in reproduction, not to usurp the process. Courts have repeatedly recognized embryos as something special….not people, but not just ordinary property either. And there are some very practical problems that could arise from a clinic or physician owning embryos. What happens if the clinic disbands? Who gets the embryos? Would the embryos be auctioned off or given to a creditor in case of bankruptcy? Would the physician’s family inherit the embryos after his death?
You have provided some techniques for California Conceptions to adopt to ensure that all embryos are owned only by patients. Alternatively, an option would be for the clinic to destroy the embryos that have not been distributed to a patient. While this would not be financially advantageous to the clinic, and some would argue is a waste of resources, it is an ethically acceptable alternative when no patients are willing to accept responsibility for the excess embryos.
California Conceptions, I urge you to join ASRM/SART. If you feel that your model is ethically appropriate, then you should be teaming up with ASRM/SART to develop guidelines for such embryo banking models, rather than shying away from industry self-regulation.
You take single sentences out of context and wrap new meanings around them. We offer both traditional embryo donation and donor/donor embryos. The website does not make a clear distinction between the two as it was written when the program was very new. We clarify all options when talking with patients as both options will be available to them. Honestly, the website needs to be updated, but that’s not the same as intentionally misrepresenting what we are doing. Patients know clearly what’s being done when they contact us and definitely know by the time they have a transfer. Fortunately, our patients are smart enough to get all of the facts before blindly following a web page. You’ve spent more time micro-analyzing the sentences than I have. I’ll be happy to consider your interpretations when we make updates as it can help make for a better webpage.
Your comments on embryo banking make it clear you haven’t read the previous posts. Egg donors are not starting medications until there are recipients there to receive them. As a result, they are not created without identified parents. You then suggest we destroy the embryos rather than match them to another couple? I hope most people reading a blog on an embryo donation website disagree with you. What happens to any embryos stored at a clinic if that clinic goes out of business? Somehow you think they go to auction or a creditor? You know better than that.
Our donors know of the donor/donor program and have the option to not participate. They can still donate for a couple needing an egg donor outside of California Conceptions.
I have initiated contact with ASRM and provided information about my program. I have also offered to provide any additional information to the committee and participate in any discussions on the topic of embryo donation or donor embryos. The meeting is not an investigation of my program by ASRM as has been suggested.
I would have time to revise the website if I didn’t have to spend so much time responding to people posting misguided opinions about what I’m doing. As I said, our patients know what we are doing and are grateful for the opportunity. That’s what is important to me.
Dr. Zeringue:
I agree that discarding any excess donor/donor embryos would not be an option I would like to see used. Would you consider having any of these embryos immediately owned by any of the recipients rather than banking them and trying to find other recipients in the future?
You describe your facility as offering both (shared/split) donor/donor embryos and the more conventional embryo donation option in which the embryos were actually donated from patients with excess cryopreserved embryos. Would you be willing to provide any statistics regarding the actual number of the two separate procedures performed in 2012? If the conventional embryo donation procedure number was substantial, perhaps some of the criticism levied would be softened by knowledge.
I agree that the ASRM Ethics Committee is meeting to discuss the embryo bank issue in general as this practice has been attempted before. It will be up to them to decide if now is the time to come out with a position statement regarding the process. If you feel singled out, I will apologize. In my recent blog, I tried to find instances where this had happened before. One must be clear, however, that your facility has (inadvertently) become a lightening rod regarding this issue and focus on your facility is inevitable given the L.A. Times article and the blogs that responded to its content.
Catherine:
You bring up some very perceptive points. Your concerns are clearly aimed at the vulnerable infertile patient.
My understanding is that the egg donors are aware of the business model the California facility is using. I have yet to see a contract so I can’t personally write on this point. Perhaps the facility would be willing to share their contracts/consents with the Legal Special Interest Group for their review. I understand the sperm donors are obtained from a national sperm bank and are probably not made aware of this potential use of their sperm from the get go. Once again, contracts/consents would need to be reviewed but my guess is that the embryo bank concept is too new and the contracts/consents probably haven’t had time to be modified.
It would sadden me to have any clinic destroy the remaining cryopreserved embryos rather than create an embryo bank. I would be torn with deciding the lessor of two evils. While a personal choice, I would tend to feel the destruction of the excess embryos would be a worse choice than creating an embryo bank, I am not sure such a decision really needs to be made. Simply making certain all the fresh and cryopreserved embryos are owned by potential recipients is all that is needed. Once done, the California facility can continue with its business plan and still maintain the highest ethical standards of medical care for their patients.
Dr. Sweet,
Thank you for initiating this conversation. The banking of embryos is a “hot” topic that needs to be considered carefully.
I must admit, I have concerns regarding the creation of embryos without a destination. Just saying out-loud, “Embryos created by a business first and then finding an intended parent second” is unsettling to me.
My field involves educating infertility patients to effectively advocate for health insurance benefits. This includes lobbying at the state and national level to ensure all infertility patients have access to the health care they need. The topic of embryos is highly sensitive within this arena and increasing the controversy to the subject does not help our efforts to secure legislative support. And while we propose infertility health benefits are pro-family, the practice of creating embryos without a prospective parent creates a factory feel rather than a gift from medical technology.
I understand the ASRM Ethics Committee will be discussing this subject soon. It is my intent to share my concerns with them and hope they will strongly consider the advocacy perspective.
Thank you again for starting this conversation.
All my best,
Davina Fankhauser
Fertility Within Reach
Davina:
Your hard work as a patient advocate is so very appreciated. I personally admire what you do for so many patients.
In defense of the California program, I don’t believe they are creating embryos first and then finding recipients second. I believe they are getting a group of recipients together to agree to use specified pair of egg and sperm donors before moving forward. Perhaps it is even possible more than one sperm donor is being used. This is no different than what is done at many programs that use a split or shared cycle protocol. My concern, however, is with the inevitable embryos that are left over from the process should an excess of fresh embryos be present after matching them to all the initially prepared recipients. Unless those excess cryopreserved embryos are owned by the recipients, an inevitable embryo bank is created by the facility with the embryos owned inevitably by the facility. This is my greatest concern.
Dr. Sweet, you must love the different tone of the responses to this post compared to the previous one. In a previous blog you made the assertion that the many negative posts seemed organized or intentional. In this blog, it’s now the opposite response and seems to be biased based on your notions of banking and ownership with a slant to your previous “designer baby” ideas. Are any of the responses here invited by you? Also, any ideas about the opinions of REI physicians?
Your topic is supposedly about embryo banking, however after many of the comments you discuss California Conceptions. I am at least happy to see that you have a more informed opinion of our services compared to the previous post. Still, much of the blog and responses are dedicated misconceptions about what we are doing. The articles you quote do not really support your arguments. The 1997 one talks a little about selecting donor characteristics but by the end it becomes clear the embryos from donor sperm and donor eggs were formed only when a recipient backed out. The doctors and embryologists interviewed didn’t seem to find this unacceptable. Of course you only quoted the attorney in the context that is suits you, but please note that that comment follows a paragraph about traditional embryo donation. She goes even further to call the process embryo adoption. Not a great post to quote here. The 2007 posts about Jenalee Ryan and the Abraham Center of Life in San Antonio, Texas have their facts wrong. Read the original articles about her program, or better yet, talk to her. Her program never started and there wasn’t a bank. The FDA showed up at her house to investigate her compliance with the FDA’s regulations. Since her service was actually a matching process between a couple using donor eggs and subsequent recipients of the left over embryos, there was nothing to investigate. Additionally, since the custody of the embryos transferred from the original couple to her customers who would pay a fee for the matching services, the program would pass your ethical test of always having an owner. Lastly, the 2012 blog by Jessica Cussins is just an uninformed rehash of your first blog. The facts are inaccurate and make accusations that are defamatory to say the least. It appears that your best references, and many of your commenters on this blog, are attorneys with an opinion and disregard for actual facts. If you want to avoid government regulation, I’d suggest you find a better circle of internet friends.
There is a trend in the comments that infer we are creating embryos “for sale” without intended parents ready to receive them and that we are storing extra embryos that we “own” and can choose to do anything with them without ethical regard to the embryos. You imply that saving embryos and matching them to another couple is still a bank and this is a bank will open up the doors for regulations and large warehouses of embryos. In making several very good points, most of which we agree upon, you are making several very big leaps and your followers have taken these assumptions at face value.
As we discussed, we differ greatly on what is a bank and what isn’t. You feel because of your “take back” policy that you don’t have a bank of embryos. In a financial bank, the bank doesn’t own the money you deposit. Is it really ownership that defines a bank? We call a sperm bank a bank because they have stores of sperm. Is there a clear owner? Wouldn’t the “bank” own them since they in turn sell the vials (presumably for the cost of procuring and processing the sperm as gametes can’t be sold)? Most people want to treat embryos differently, and ASRM holds that embryos should be afforded a higher degree of moral responsibility. By pushing the topic of ownership and banking, your message may actually become more inviting of regulation and political attention that you intend. Our actions are in compliance with ASRM and you are the one insisting on labels of banks and ownership. Do you not think that there are people that will be happy to call your stores of patient-owned embryos a bank? This would give more fuel to the “personhood” advocates than my program that utilizes all of the viable embryos – as opposed to freezing indefinitely or discarding them.
You also imply that a bank that owns embryos is free to make any decision they want. We are following the guidelines that embryos are afforded a higher ethical standard and the only option for any embryos not transferred in a fresh cycle is to be transferred to another recipient couple. Is it necessary to label the embryos with an owner if we afford then the same ethical custodianship we would with any other embryo?
If embryos are to be treated with more than just a higher ethical standard, should we reduce them to property that is owned with a title or license issued to the parents? That is the slippery slope of your argument. Ideally we would all want to avoid such a thing.
Clinics everywhere encounter extra embryos as part of the pursuit of helping couples have children. The fertility community has deemed it morally acceptable to freeze hundreds of thousands of embryos that remain in storage year after year. This is considered ethical because someone “owns” them and can decide what to do with them. The most common option is to discard them. In our program, any embryo suitable for transfer is transferred. If there is an excess of frozen embryos, donors are not scheduled for a fresh cycle until there is a need for a fresh donor cycle. The program isn’t discarding embryos, yet you would find this somehow less ethical because someone doesn’t “own” the embryos.
I would suggest you focus less on your labels and more on the actual ethics of the actions. Less on the potential abuses and more on the facts of what is being done. Does the state own orphans? Do parents own their children? I think the thought of that would offend most parents. We have a responsibility and an obligation to them. So if we must own an embryo, do we give up ownership at implantation? My point here is the label of ownership itself invites regulation, while transferring all available embryos to fully informed recipients demonstrates compliance with an ethical obligation to the embryos consistent with a custodianship rather than ownership.
Just to be clear, fertility clinics have an ethical responsibility to treat embryos with a high regard for the potential people they represent. We are doing this without a doubt, and all of our viable blastocysts are transferred.
Your promotion of the term “embryo creation” is not advised as the term is borderline offensive. I would imagine most REI’s would feel that we are humble in our profession and actually are simply arranging the meeting of the sperm and egg followed by the meeting of the embryo and the uterus. Creation implies something entirely beyond our scientific understanding. Since donor sperm and donor eggs are being used, “donor embryos” is an acceptable term to distinguish the embryos from traditional “donated embryos”. Keep in mind that California Conceptions also has, and receives, donated embryos similar to your program. I agree our website is in need of updating as it’s not had any significant changes since the program was first introduced.
In regards to your statement “If all the cryopreserved donor/donor-conceived embryos find a home, I have less to complain about. What happens, however, if some of the cryopreserved embryos are never chosen? Who will decide their fate? Who should decide their fate?” I think you have less to worry about. You should have a very clear idea of the shortage of embryos available for traditional embryo donation, let alone embryos with a high potential for pregnancy. There aren’t embryos that do not get transferred in our program. Can you think of a scenario in which gametes from an egg donor and a sperm donor would produce a blastocyst that is not desirable? We are even transferring day 5 morulae with excellent results.
There are several very good points that most practitioners would agree upon. These will be the topics of ASRM’s discussion, and it’s not accurate to attempt to portray the upcoming meeting as some form of investigation of California Conceptions. I’m happy to discuss my program with ASRM and they are aware of this. As members, you and I will likely have an opportunity to comment on their opinion and suggest changes before it is published. I would imagine any published opinion would be in the form of a revision of the 2009 opinion on embryo donation – assuming of course they feel the need to publish an updated opinion. Getting into topics of ownership and treating embryos different from gametes could risk the types of attention none of us want. I’m confident what you want is ethical agreement and not government regulation of reproductive property, but some of your arguments are headed in that direction.
I do appreciate that this blog was much more thought through than the previous blog. Hopefully some of the commenters here can review my previous responses and refrain from making false assumptions about what we are doing. Even with news stories about IVF, there are plenty of people posting very strong opinions and disagree with any form of assisted reproduction. It’s not surprising that there are differing opinions about donor embryos and donated embryos. It’s good to voice these opinions, but care should be given to not wrongly accuse a program of doing something they are not doing.
Ernest Zeringue MD
California IVF Fertility Center
California Conceptions Donor Embryo Program
Dr. Zeringue:
I know you are aware that I did ask many people in the ART world to comment on my most recent blog. I also asked them to agree or disagree and I have not blocked any comments made thus far,including your own. I actually rarely block comments unless they are unrelated or inappropriate as I feel open discourse is so necessary to the quality of this blog.
I would agree that the physicians and embryologists have been relatively silent on the topic with respect to leaving comments. I suspect that they do not like to get embroiled in controversy much less disagreements that may occur between practices. Both myself and my embryologist have heard from a number privately but not here on the blog.
“My circle of internet friends” are my peers who do not hesitate to tell me when I am off base. Their opinions are their own and I could never force them into a perspective as they are far too independent in thought and personality for that.
It would appear that you are now stating that donor sperm + donor eggs = “donor embryos” and that this should be distinguished from “donated embryos.” That is an interesting point, indeed. I would have to defer to others regarding this distinction. I can’t think of another set of ART words that are so similar to each other that mean two totally different things. At the very least, I would be concerned that the general public will be unaware of the differences but perhaps they could be educated.
In reality, this is not the first time that this type of wordplay has taken place. The first “embryo donation” procedure that is often quoted (A Trouson et al. Pregnancy established in an infertile patient after transfer of a donated embryo fertilized in vitro BMJ 1983;286:835-8.) was actually a shared cycle with the first couple going through ART gave a fresh embryo to a 42 y.o. woman that happened to have an LH surge on the appropriate time. A trisomy 9 was the final result. I don’t think we really know when the first true “embryo donation” procedure actually took place, as defined by ASRM and contemporary literature. By your definition of “donor embryos,” I suspect the first case was probably in the middle 80’shortly after egg donation was first successful. I am unaware if your definition “donor embryos” is being commonly or currently used in literature or ART facilities.
As I have written, there is no angst between us. I’m not sure we have ever met although I did try to reach out to you, but never had a return phone call, after the first blog. I have stated that I feel your intent has been honorable and your goals patient-centered. You are offering a unique option that is more affordable than many others. My primary concern is the creation of an embryo bank, small or large, who owns the embryos and the unintended consequences that may follow. The ASRM Ethics Committee will hopefully take the topic up and I am certain they will look well beyond your practice in making their decisions.
If not actively resisted, the creation of embryo banks by other programs will certainly occur, except in New York where it is banned, as the financial incentive is simply too great for practices to resist. Your business model may morph into something less acceptable to both of us and the only option that I see to slow the movement towards the creation of embryo banks is for the Ethics Committee to make a clear and concise determination regarding the issues I have brought up and perhaps others that they feel I have missed. Once done, this will hopefully be enough to slow or stop the momentum towards embryo banks or the next probable outcome will be legislative events, for which we will all have minimal control.
The real difference between the California Conceptions program and traditional IVF treatments is that with California Conceptions ALL viable embryos are implanted and given the chance to become a baby either immediately or within a very short period of time (usually less than 60 days), whereas in traditional IVF programs a select few are implanted and the remaining are either frozen indefinitely, destroyed, or donated to science. So my question to you is: What embryo would you rather be? The one “owned” by a clinic but destined to have a chance to become a baby or the one “owned” by a patient but destined to be forever frozen?
“I suggest that any remaining embryos be owned by one or more of the recipients and the entire cycle should not move forward until at least one patient agrees to take the extra cryopreserved embryos, should any exist.”
So what you are essentially suggesting is to turn CC into a traditional program where most embryos are frozen indefinitely and have no chance at life. I find that very sad.
I am curious where you get your information regarding how long it takes for any residual cryopreserved embryos to find a home. You state that all are transferred within 60 days. What will happen if the embryo combination is not desired? What happens when this process continues to be done on an even larger scale? What happens when other practices perform the same process creating embryos in mass awaiting a home?
You may an excellent point that the embryos should have a chance at life. I agree this is true for all cryopreserved embryos. If half of the cryopreserved embryos are not use for reproduction by the individuals who created them, we have a great deal of work to do for the remaining frozen embryos to be used for good. Potentially increasing the number of embryos cryopreserved does nothing to rid us of this problem but only potentially complicates the issues.
The fundamental questions is who should own embryos. If practices are able to create embryo banks, then that is precisely what will be done. The financial advantages are simply too tempting. If this is done at other locations, it is only a matter of time before a facility will go out of business or that has a host of embryos are found languishing in cryopreservation.
At the risk of repeating myself, a physician or facility should not own embryos, no matter how good their heart is. If thousands of embryos are owned by IVF facilities and recipients are not found, what do you expect those pro-life individuals to do with that issue? I feel there could be a political backlash that could influence reproductive care for so many.
I would not assume that the embryos will find a home if owned by a facility. One does not make the other certain.
Thank you again for your comments.
[…] Unlike the IVF client who decides what to do with the embryos created from their own gametes, this clinic decides what to do with the “product” it creates. This is making many people uncomfortable. One doctor who works in the field considers it tantamount to being a “McEmbryo.” […]