Posts Tagged ‘IVF’
Why Creating “McEmbryos” is Just Plain Wrong
Introduction
Recently, Alan Zarembo of the L.A. Times released a story alleging that California Conceptions was combining donated eggs with donated sperm and called them “donated embryos.” If there were leftover cryopreserved embryos, ownership of the embryos apparently went to California Cryobank (CC). If true, this is an egregious assault on reproductive ethics.
Defining embryo donation
About one-third of all patients undergoing in vitro fertilization (IVF) will have excess embryos to cryopreserve. About one-half of these will not be used for reproduction by the patients who created them. (Bangsboll et al., 2004; Lyerly et al., 2010) Embryo donation occurs when patients with unused cryopreserved embryos make the amazing decision to pay it forward and donate their embryos to patients in need. In true embryo donation, the patients own the embryos and make disposition decisions regarding their embryos. It is estimated that 2-10% of all cryopreserved embryos are donated to patients in need.
Why is creating “McEmbryos” so wrong?
Allegedly, California Conceptions would use donor sperm and donor eggs to create embryos. At times, all the resulting embryos would be transferred simultaneously to numerous couples, each receiving approximately two embryos at a time. This would commonly be called a “split donor/donor cycle.” It is, however, an absolute misrepresentation to call them donated embryos. At least in this split donor/donor cycle scenario, where all the embryos were transferred, there would be no cryopreserved embryos left whose ownership was uncertain.
What if not all the embryos were transferred and some were cryopreserved? As I understand, CC transferred no more than two embryos at a time to numerous patients, with the remainder cryopreserved. The residual cryopreserved embryos became the property of CC.

According to the article, egg and sperm donor profiles are sent to prospective recipients. As soon as CC received a “buy-in” from a few patients, the “donor embryos” were created from the donor eggs and sperm. Who made the decision to combine these two donors? What happens to the left over cryopreserved embryos? The article stated that dozens of embryos would be created through the combination of a pair of donors with the embryos then frozen while CC looked for patients who wanted them. And yet, the clinic claimed to have only ten sets of cryopreserved “donated embryos” in their tanks at any given time.
While they stated they didn’t want to create a bank, it would appear that this is precisely what was being done.
I feel there is a potential conflict of interest on the part of any IVF facility regarding the disposition decision of any cryopreserved embryos that they own. Patients normally have options such as using them to build their family, donation to science, donation to a laboratory for quality assurance testing and personnel training, keeping them cryopreserved forever, and finally, donating them to patients in need (embryo donation).
With the methods described in the article, a number of logistical and ethical questions arise:
- Were the sperm and egg donors fully aware of what was to be done with the resulting embryos?
- How did the IVF practice decide which sperm and egg donors should be combined? Was this decision made through market research? If so, who made these decisions?
- Is anyone tracking where all these donor-donor conceived offspring end up?
- Who ultimately owns the cryopreserved embryos? In the article, the physician interviewed said the clinic owned them when they were frozen
- Who makes the disposition decisions regarding these embryos? Will the IVF facility that owns the embryos be likely to make disposition decisions that do not benefit their bottom line? Who has the best interests of the cryopreserved embryos at heart when the embryos are owned by the IVF facility? Is it possible that CC is the entity that is really “donating” their remaining cryopreserved embryos
- What happens to the cryopreserved embryos if the practice closes or is sold?
- Perhaps most important, although it may not be a problem presently but for the future, what happens to the cryopreserved embryos that are never chosen?
While certainly not meaning to demean the cryopreserved embryos, I can’t help but think of these dono/donor cryopreserved embryos as fast food embryos or “McEmbryos.” I can just see the patients coming in, looking above the cash register to the menu above and ordering a “Number 3,” which has a burger (i.e., bright, blonde-haired, blue-eyed egg donor) and fries (i.e., handsome, athletic and tall sperm donor) and ends up getting the order supersized to boot (i.e., requesting twins). I should write clearly that this is not the current method CC uses to to match recipients to remaining cryopreserved embryos but the slippery slope exists and other practices may eventually emulate this process
What did EDI try to do over the past year to remedy the problem?
We suspected what might be happening at CC well over a year ago but didn’t have proof. We approached the American Society for Reproductive Medicine (ASRM) who examined the information and eventually sent it on to the Society for Assisted Reproductive Technologies (SART). SART did an investigation agreeing with our preliminary assessment. Unfortunately, CC was not a member of SART so they had little influence with CC.
There was some discussion of placing CC on the Center for Disease and Control’s (CDC) radar, asking that they potentially audit CC. I am not aware if this was ever done.
There was some discussion of revising the Ethic’s Committee Opinion on embryo donation detailing the inappropriateness of creating “McEmbryos,” but in the recent revision sent out to all ASRM members to review this past August contained no such language. I contacted ASRM and volunteered to help write the couple of paragraphs that would address the issue but I was never contacted. My current understanding is that the ASRM Ethics Committee will be taking up this issue in the beginning of 2013 and I am hopeful they will make a stand against creating “McEmbryos.”
Is it really ASRM or SART’s fault?
ASRM and SART are membership organizations. Anyone can join ASRM whereas SART is only open to IVF practices. These entities are not designed to truly police their members. Certainly, they can bar them from membership, but let’s face it, this is really not much of a punishment. Most patients are not really aware if a practice is a member of either organization, so expulsion does more to protect ASRM and SART from criticism than it does to protect the patients.
In reality, I am not suggesting that ASRM or SART begin sanctioning their members. These organizations are made up of bright individuals wanting what is best for members and patients alike. I don’t believe ASRM or SART could ever expose themselves to legal liability and try to be anything more than what they were originally designed to be.
I feel criticism towards ASRM and/or SART is potentially misplaced. While I do feel these organizations can certainly take a stand against the creation of “McEmbryos,” they can only provide educational materials and information to members and patients. never entering the realm of fining, condemning practices or policing practices. That is simply not their job.
I am not being insensitive to the needs of the patients
California Conceptions is providing amazingly healthy embryos to patients in need. How could anyone not be touched the story twin girls born to a single 41 year-old woman? There is no question that the donor/donor split cycle can be far more cost effective than many other options. The ends to this process are what we all strive for – a healthy family.
Call me old-fashioned but I still feel there are instances where the ends cannot justify the means. Are we are loosing all respect for the embryos and treating them utterly as a commodity? The slippery slope is becoming quite steep. Are we ready for expanding banks of unclaimed embryos across the country owned by practices or physicians and not the patients? I’m sorry but the means being used here are fraught with uncertainty and may result in a list of unintended consequences.
What are the potential repercussions of the L.A. Times story?

At least this election year is over. I had grave concerns that the story would break early in the election cycle and would become a political football, resulting in a series of consequences around the country. I still believe we are at risk in the following ways:
- • Poorly designed and reactive legislation may yet be created on state or national level
- • This story may motivate the “Personhood” advocates by encouraging them to win personhood for embryos thereby protect them from becoming “McEmbryos”
- • There will be “guilt by association,” leaving other legitimate embryo donation facilities open to criticism and ridicule
- • All of this will reflect poorly on basic IVF facilities that are frequently viewed as unregulated, even though we are accountable to more regulatory agencies than any other area of medicine
There may be significant backlash regarding this story and we should all be prepared to answer questions that may arise from the media, our peers and our patients.
How can embryo donation programs hold but not own the donated embryos?
At Embryo Donation International (EDI), the embryo donors are still able to request that their donated embryos be returned if needed. For example, if the children of an embryo donor were tragically killed in a motor vehicle accident, it seems absolutely appropriate that the cryopreserved donated embryos should be sent back to the donors. To discourage this from being done without good reason, transportation costs for returning the embryos, which is estimated to be $300, are the responsibility of the original donors.
Once the embryos are transferred into the recipients, however, they now “own” them. In this way, EDI never truly owns the donated embryos. We are the conservator and protect the embryos while never making any disposition decisions regarding their fate. We never own the donated embryos and we encourage all embryo donation facilities adopt this model of conservatorship.
What can be done to correct the current problem?
- Various membership organizations such as ARSM, Pacific Coast Fertility Society (PCFS), SART and RESOLVE could release position statements condemning the creation of “donated embryos” without a destination. This could help guide public opinion.
- Perhaps the embryo donation programs would be willing to sign a contract stating that they will not participate in the creation of embryos without a destination. Programs willing to sign and honor the contract would be adhering to the highest of ethical standards.
- Through the court of public opinion and if the L.A. Times article is accurate, patients may no longer want to participate in what they feel in an unethical practice.
- Legislative action on the part of California may be necessary but this will take time and a great deal of expertise. We run the risk, however, of having well-meaning legislative actions spilling over and harming the process of embryo donation or IVF itself.
- CC itself may need to modify its business model by allowing patients to own the cryopreserved embryos.
From my perspective, we have a few options:
Something really needs to be done. I don’t feel that this unethical practice should continue. A corporation, business or physician practice should never own embryos, no matter how brief. These embryos are also not truly donated unless you feel CC is able to donate the excess cryopreserved embryos. The question is if we should play an active or a passive roll in determining what takes place. I personally prefer the active roll so you can count EDI in on doing our best to guide the process.
Sour grapes? Nope, just sour taste!
CC is a potential competitor of EDI. I have made this clear to each and every person I have spoken to regarding this current dilemma. When we were contemplating the expansion of our ten-year embryo donation program into EDI, we also looked at the option of a money-back guarantee such as is offered by CC. Understanding the delivery rates for recipients of truly donated embryos ranges from 27-45%, the likelihood of returning the majority of the payments back to recipients made it unlikely we could even keep our doors open. Most “shared risk” options also charge a premium on top of the normal fees. Recalling that embryo recipients are emotionally and financially drained, the idea of tacking on a large additional fee seemed unfair to the recipients and quite impractical to the process. Embryo donation works for recipients, in part, because it is more cost-effective than many other options.
So you see, it is not “sour grapes” that is guiding my writing; it is just a sour taste. If the article was accurate, I feel strongly that creating “McEmbryos” is an affront to IVF and embryo donation programs, misleading to embryo recipients and totally unfair to the cryopreserved embryos that are currently waiting to be chosen.
If you agree, please co-sign this blog….
We are going to do something a bit different with this blog. We are strongly encouraging not just the routine comments that follow our blog but we are also asking that practices, patients and interested parties who agree that creating “McEmbryos” is ethically inappropriate sign below. By endorsing the statement below, we will hopefully begin to separate ourselves from such entities that practice the “McEmbryo” method of “embryo donation,” moving forward with a resolution that will work best for all.
routine comments that follow our blog but we are also asking that practices, patients and interested parties who agree that creating “McEmbryos” is ethically inappropriate sign below. By endorsing the statement below, we will hopefully begin to separate ourselves from such entities that practice the “McEmbryo” method of “embryo donation,” moving forward with a resolution that will work best for all.
By signing below, I do hereby agree that creating banks of cryopreserved embryos is ethically unjustifiable and support sound solutions that will adhere to the highest of ethical standards supporting patients and cryopreserved embryos in the best possible way.
References:
What Impacts Embryo Donation Success Rates?

Craig R. Sweet, M.D.
Reproductive Endocrinologist

Corey Burke, B.S., C.L.S.
Laboratory Supervisor
Introduction
Asking what determines the success rates in embryo donation is an excellent question. The answer, as one might expect, is neither simple nor completely understood.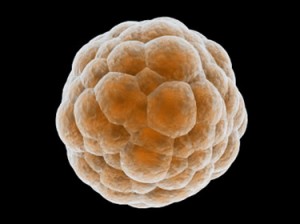
Embryologists and physicians try to choose the fewest number of healthy embryos for fresh transfers to increase success rates while minimizing multiple pregnancy rates. It is indeed a delicate balance. For example, it is well understood that in Europe, physicians transfer fewer embryos but patients also suffer significantly lower success rates than in North America. (Boostanfar R, et al. Fertil Steril 2012)
What variables do we examine to estimate probable success?
Since donated embryos are cryopreserved, the variables become even more complex compared to fresh embryos. In combining a great deal of published data and over 20 years of IVF and embryo transfer experience, we came up with what we feel are the variables which seem to influence success rates:
| Very Important! |
Preferred |
Less Optimal |
| Did the fresh cycle in which the embryos were frozen result in a pregnancy & delivery? |
Successful pregnancy and delivery |
Fresh transfer resulted in miscarriage or no pregnancy |
| Number of embryos available in a given donated set |
Four or more |
Three or fewer |
| Past implantation rates of both fresh and frozen embryo transfers |
High implantation rates |
Low implantation rates |
| Quality of the embryos frozen (link) |
High quality (Blastocyst) |
Medium quality |
| Age of the women when the eggs were provided to create embryos |
Less than 35 years old |
35 years of age or older |
| Overall health of the embryo recipient (link) |
Healthy |
With treated or untreated medical issues |
| Important |
Preferred |
Less Optimal |
| Stage of growth when the embryos were frozen (link) |
Day 5, blastocyst stage |
Day 3, 8-cell stage |
| Technique used to freeze/thaw or vitrify/warm the embryos (link) |
Vitrification |
Slow freeze |
| Overall frozen embryo transfer pregnancy rates for facility freezing the embryos |
30% or more |
Less than 30% |
| Overall frozen embryo transfer pregnancy rates for facility thawing the embryos (EDI) |
High at 30% or more |
Less than 30% |
| Ejaculated vs. surgically aspirated sperm used for fertilization |
Ejaculated sperm |
Surgically aspiration sperm |
| Somewhat Important |
Preferred |
Less Optimal |
| Was preimplantation genetic testing of the embryos done? |
Yes |
No |
| Age of the male producing the sperm |
Less than 40 years old |
More than 40 years old |
| Past successful deliveries with other embryos from donating facility |
Yes, with past deliveries |
Miscarriage, reduced survival of embryos or failed implantation |
| Probably Unimportant |
Preferred? |
Less Optimal? |
| Cryopreservation duration |
Less than 10 years? |
More than 10 years? |
The above variables influence EDI’s decision to both accept embryos from other facilities as well as determine how many donated embryos should be thawed/warmed to achieve a successful delivery.
The importance of the embryo recipient’s health should not be underestimated
In a previous blog, we described how important it was for our embryo recipients to be healthy. (link) Inadequately treated health problems, harmful medications, recreational drug use as well as smoking and weight concerns all play a potential role affecting success rates. It is clear that success depends on both the quality of the donated embryos and the overall health of the recipient.
Are all donating IVF facilities the same?
We understand that not all IVF facilities have the same success rates. Some facilities will have provided EDI  donated embryos with consistently high implantation rates while others may provide embryos of consistently lessor quality. EDI examines a facility’s past fresh and frozen embryo transfer pregnancy rates as well as its past history of providing EDI with donated embryos. It does, however, take a fair amount of time to seemingly identify a trend but we endeavor to examine all the variables we can. Our contact management database system was recently upgraded to track these variables more consistently.
donated embryos with consistently high implantation rates while others may provide embryos of consistently lessor quality. EDI examines a facility’s past fresh and frozen embryo transfer pregnancy rates as well as its past history of providing EDI with donated embryos. It does, however, take a fair amount of time to seemingly identify a trend but we endeavor to examine all the variables we can. Our contact management database system was recently upgraded to track these variables more consistently.
Do your embryos make the grade?
Understanding that all of the above variables are quite complex, we endeavored to find a simple way to convert the data into something patients could more easily understand. Since nearly all patients understand the basic A, B & C grades we used to receive in school, we modeled our grading of the embryos around these letter grades.
We created a mathematical model to assess a number of the above variables, converting the final analysis to A+, A, A-, B+, B and B- letter grades. Interestingly, we found the model really did help to predict delivery rates and continue to use it to this day to grade individual embryos as well as entire sets of donated embryos.
What information do we gain on the day of thaw and embryo transfer?
Most frequently, the embryos are thawed just hours before transfer. At times, we may thaw them days prior if, for example, they were frozen early in their development and we want to grow them further before deciding how many to transfer. Therefore, the following last set of variables will also influence success rates:
| Important |
Preferred |
Less Optimal |
| Survival rates of thawed embryos |
100% |
Less than 100% |
| Overall appearance of the thawed embryos |
Healthy, expanding and growing |
Evidence of cellular damage |
If 100% of the embryos, perhaps three out of three, survive the thaw and look healthy, we feel this is a good sign. If only 50% survive, for example perhaps only two of four, then we are concerned that the overall implantation rates will be reduced and that we might need to find more embryos to transfer just to get to the “finish line” of pregnancy and delivery. Ultimately, we want at least two high-quality embryos or up to four less certain quality embryos placed on the day of transfer.
What are the national success frozen embryo transfer delivery rates?
 In 2009, the CDC reported that there were 26,069 frozen embryo transfers performed in the U.S. with an average delivery rate of 31% per embryo transfer procedure. In addition, there were 6,074 frozen embryo transfers using embryos created from donated eggs (i.e., younger women) with slightly higher delivery rates of 34%. Please recall that donated embryos generally come from the very same types of patients listed in these success rates.
In 2009, the CDC reported that there were 26,069 frozen embryo transfers performed in the U.S. with an average delivery rate of 31% per embryo transfer procedure. In addition, there were 6,074 frozen embryo transfers using embryos created from donated eggs (i.e., younger women) with slightly higher delivery rates of 34%. Please recall that donated embryos generally come from the very same types of patients listed in these success rates.
What are EDI’s success rates?
We do our best to screen the embryos, carefully trying to choose the embryos most likely to implant. We estimate delivery rates with donated embryos to range from 27 – 42%, depending on the many variables listed in this blog, with a multiple pregnancy rates of 20-25%. We wish the success rates were higher, but please understand that frozen/thawed embryos implant and grow less frequently than fresh embryos and these percentages are entirely consistent with the frozen embryo transfer success rates described in 2009, which ranged from 31-34%.
Even with the slightly lower delivery rates compared to fresh embryo transfers, embryo donation remains one of the best and most cost-effective options for patients who cannot otherwise afford egg donation or qualify for adoption. Embryo donation still allows a woman to experience pregnancy and delivery while bonding, nurturing and protecting the ongoing gestation.
Summary
There are many variables that go into determining the potential success rates for a given set of donated embryos. First, we attempt to examine these variables carefully in deciding if EDI will accept the donated embryos. Second, we use this same information to determine how many embryos we should thaw/warm and eventually transfer. The process remains a bit of an ART (pun intended) since the complete understanding of how all of these variables influence each other and the ultimate success rates are yet to be fully known.
References
“Annual ART Success Rates.” Centers for Disease Control and Prevention. Division of Reproductive Health, 19 Apr. 2012. Web. 24 Apr. 2012. <http://www.cdc.gov/art/ARTReports.htm>.
Boostanfar R, Mannaerts B, Pang S, Fernandez-Sanchez M, Witjes H, Devroey P; Engage Investigators. A comparison of live birth rates and cumulative ongoing pregnancy rates between Europe and North America after ovarian stimulation with corifollitropin alfa or recombinant follicle-stimulating hormone. Fertil Steril. 2012 Mar 27.